Maintaining a current Investigator’s Brochure (IB) is a fundamental component of ensuring clinical trial safety. The IB is a dynamic document that must evolve to reflect new clinical and nonclinical data gathered about an investigational product. This systematic process is a regulatory requirement and essential for trial integrity.
The Critical Role of IB Updates and Control in Clinical Trials
The Investigator's Brochure serves as the foundational document for patient safety and informed consent in a clinical trial. As defined in the ICH E6 Good Clinical Practice (GCP) guidelines, the sponsor is responsible for providing investigators with the most current and complete information available on a product. This ensures that clinical decisions, risk assessments, and discussions with trial participants are based on a comprehensive understanding of the investigational product's profile.

This responsibility has grown in complexity. Over the past decade, the average size of IBs has increased significantly. A small molecule IB that might have been 60–80 pages is now often 150–250 pages for biologics and advanced therapies. This growth reflects regulatory expectations for the integration of extensive data. For additional context, the Colorado State University research site provides insights into this evolution.
Why Documentation Control Is a Regulatory Imperative
Ineffective documentation control for an IB presents a direct risk to trial integrity and patient safety. An outdated IB at an investigative site means clinicians may be unaware of new safety signals or critical shifts in the risk-benefit profile. This information gap can lead to mismanagement of adverse events or flawed informed consent discussions.
From a compliance perspective, regulatory authorities such as the FDA or EMA require a clear, auditable trail for every version of the IB. Inspectors will examine:
- Version History: A complete log of every change, with clear justification for each update.
- Controlled Distribution: A documented system demonstrating that every investigator, site, IRB/IEC, and relevant health authority received the correct version in a timely manner.
- Acknowledgment of Receipt: Verifiable proof that investigators received and reviewed the updated safety information.
The absence of such controls is a significant compliance issue for regulators.
Core Components of a Compliant IB Management Process
A compliant management process is built on several essential components. These elements work in concert to ensure the IB is accurate, current, and correctly distributed. A failure in one area can lead to systemic compliance issues.
The table below outlines these core components and connects the process to its underlying regulatory and operational purpose.
Core Components of a Compliant IB Management Process
| Process Component | Regulatory Rationale (ICH E6) | Operational Goal |
|---|---|---|
| Governance & SOPs | Establishes sponsor responsibility for maintaining an accurate and current IB. | Define clear roles, update triggers, and approval workflows to ensure consistency. |
| Change Control | Mandates that new information is reviewed and incorporated as necessary. | Create a structured process for proposing, reviewing, and implementing changes. |
| Version Management | Requires that the IB is reviewed annually and revised when new data is available. | Maintain a clear, auditable history of every document iteration and its distribution. |
| Distribution & Tracking | Ensures investigators are informed in a timely manner of relevant new information. | Guarantee and document that all sites receive the correct IB version promptly. |
These processes collectively support the creation of a single, reliable source of truth for the product's safety information.
The objective of rigorous investigator’s brochure updates and documentation control is to create a single source of truth for product safety information. This unified approach protects participants, supports investigators, and provides verifiable proof of compliance during regulatory inspections.
Building Your Framework for Governance and Change Control
Effective IB management requires a structured system rather than a reactive process. A proactive and well-documented framework ensures that each update is predictable, precise, and audit-ready.
This system is formalized in a Standard Operating Procedure (SOP), which serves as an operational blueprint. The SOP eliminates ambiguity by defining every step from the initial update trigger to final distribution and archiving.
Who Does What? Defining Roles and Cross-Functional Responsibilities
Ambiguity in role ownership is a common cause of delays and errors in the IB update process. A sound governance model establishes a cross-functional team with specific responsibilities assigned to each member.
A typical team structure includes:
- Authors & Medical Writers: Responsible for drafting content and integrating new data from multiple sources into a scientifically accurate narrative.
- Medical Reviewers (Physicians): Accountable for the medical accuracy of the content, particularly the Reference Safety Information (RSI), and for assessing the clinical impact of changes.
- Safety & Pharmacovigilance Experts: Responsible for analyzing safety signals and adverse event data to ensure the IB reflects the latest understanding of potential risks.
- Regulatory Affairs Specialists: Ensure the IB and its updates comply with global regulatory guidelines (e.g., ICH, FDA, EMA) and manage submissions.
- Final Approvers: Senior leadership or a dedicated Safety Management Team that provides the final sign-off, confirming the updated IB has passed all reviews.
This structure creates a clear chain of accountability, which is essential for audit purposes.
Pinpointing the Triggers for an IB Update
An effective SOP specifies the events that initiate an IB update, removing guesswork from the process. While ICH E6 mandates an annual review, other critical events should also trigger an update.
The core principle of a strong governance framework is proactivity. The system should anticipate regulatory expectations by pre-defining every trigger, role, and workflow involved in managing investigator’s brochure updates and documentation control.
The SOP should list triggers such as:
- Significant New Safety Information: The discovery of a new serious adverse reaction or a notable change in the frequency or severity of known risks must trigger an immediate review.
- The Annual Review Cycle: The mandated yearly review is a non-negotiable checkpoint to confirm the document's accuracy and relevance.
- New Preclinical Data: Findings from long-term toxicology studies or other nonclinical research can alter the understanding of a product’s safety profile.
- Changes in Product Formulation: Modifications to the manufacturing process or composition that could impact pharmacology or safety necessitate an IB update.
Mapping Out Your Change Control Workflow
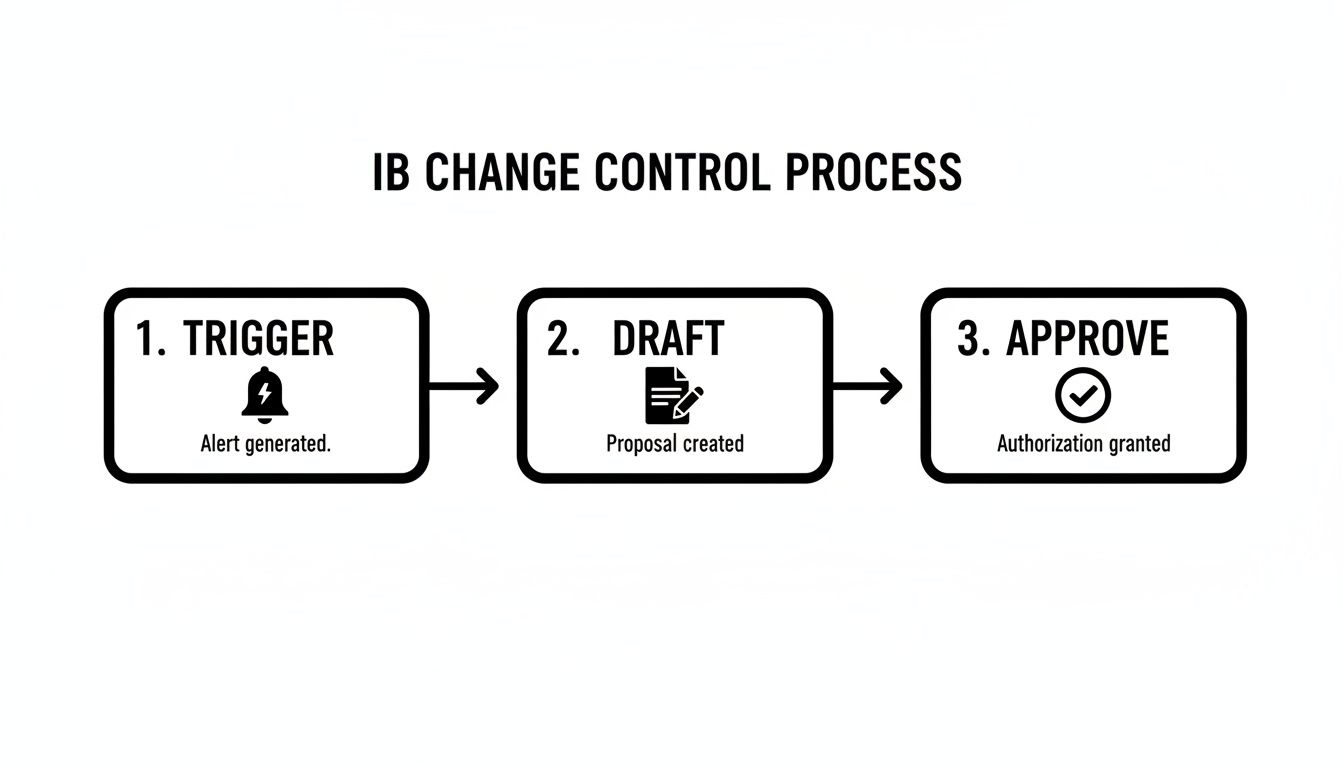
A meticulously defined change control process is essential for maintaining an auditable trail of every revision. This workflow ensures that each proposed change is systematically reviewed, justified, approved, and documented before implementation. For further information, you can explore our guide on change control in clinical trial documentation.
The process map should trace the document’s journey from an initial draft with marked changes (e.g., redlines) through review cycles where experts provide feedback. After consensus is reached, the document proceeds to final approvers. The new version becomes official only after a locked, timestamped approval is secured. This controlled, sequential process is foundational to good investigator’s brochure updates and documentation control.
Executing Flawless Versioning, Auditing, and Distribution
Once the governance framework is established, the focus shifts to the mechanics of version control and compliant distribution. For investigator’s brochure updates and documentation control, a complete, auditable history of every version is essential for inspection-readiness.
This requires tracking every draft, redlined change, and final approved document. Each version needs a unique identifier (e.g., Version 4.0 for a major annual update, Version 4.1 for a minor correction) and a summary of changes. This detailed record-keeping provides inspectors with a transparent view of the document's lifecycle.
Maintaining an Impeccable Audit Trail
The audit trail is a primary defense in an inspection. It must demonstrate who did what, when, and why. For any IB update, the trail must capture:
- Change Initiation: The trigger for the update and the date.
- Review Cycles: All comments and resolutions from every reviewer (medical, safety, regulatory), with timestamps.
- Final Approval: The electronic signature and date from the final approver, which locks the document.
- Superseded Versions: A clear log showing which version was retired and the effective date of the new version.
This historical log is critical for addressing questions about the state of knowledge at a specific point in a trial. For more detail, refer to these version control best practices for clinical trial documents, which explain how to build such systems.
The Critical Distribution and Acknowledgment Loop
Approving an updated IB is only one part of the process. Ensuring its timely distribution to the correct recipients and documenting receipt is equally critical. The distribution process must guarantee that every investigator, study site, and IRB/IEC receives the correct, final version without delay.
Manual systems relying on email and shared drives are prone to failure. Spreadsheets become outdated, emails are missed, and assembling a distribution log for an auditor can become a significant challenge.
A common and avoidable inspection finding is the failure to document that investigators have received and acknowledged the latest safety information. A closed-loop system that automates distribution and captures acknowledgments transforms this high-risk activity into a routine, auditable process.
The change control process, from trigger to sign-off, is a structured workflow preceding distribution. Each step is part of a broader quality management system.
A dedicated documentation platform can automate this entire loop by distributing the new IB to a pre-defined list, tracking delivery, and capturing electronic acknowledgments. This creates a real-time, verifiable record of compliance with GCP requirements to keep investigators informed.
Regulatory bodies take this seriously. Deficiencies related to essential documents are cited in approximately 10–20% of GCP inspection findings, many of which stem from poor version control and failure to document receipt of new safety information.
IB Version Control and Distribution Methods Comparison
The table below contrasts manual methods with a modern, platform-based approach, highlighting differences in efficiency and compliance risk.
| Activity | Manual Process (Email/Shared Drives) | Platform-Based Process | Regulatory Risk |
|---|---|---|---|
| Versioning | Inconsistent file naming; risk of using outdated versions; manual logs | Automated version numbers (e.g., 5.0, 5.1); automatic archival of old versions | High |
| Audit Trail | Manually compiled from email chains; often incomplete or hard to follow | Automatic, timestamped log of all actions (views, edits, approvals) | High |
| Distribution | Manual emailing to a distribution list; high risk of human error | Automated, role-based distribution to all required stakeholders at once | Low |
| Acknowledgment | Manual tracking in spreadsheets; chasing individuals via email | Automated reminders and electronic acknowledgment capture; real-time dashboard | High |
| Inspection Readiness | Time-consuming assembly of records to prove compliance | Instant generation of comprehensive, audit-ready reports | Low |
Systematizing versioning, auditing, and distribution allows sponsors to provide inspectors with clear, undeniable proof of compliance, mitigating the risk of outdated safety information being used at clinical sites.
Weaving Your IB Updates into the TMF and Regulatory Fabric
Managing the Investigator’s Brochure is not an isolated activity. Each update has implications for the Trial Master File (TMF) and can trigger other regulatory obligations. Failures in investigator’s brochure updates and documentation control at this stage can compromise the inspection-readiness of the entire study.
The TMF is the official record of a clinical trial. ICH E6 guidelines mandate that it must contain a complete and current history of all essential documents, including every version of the Investigator’s Brochure. When a new IB is approved, filing it promptly and correctly in the eTMF is a fundamental compliance requirement.
Keeping Your TMF Healthy and Ready for Inspection
An eTMF containing an outdated IB is a significant finding for an inspector. Regulators expect to see a clear, chronological record demonstrating that the IB version in the TMF matches the version distributed to and acknowledged by clinical sites.
This alignment is non-negotiable. An inspector will cross-reference eTMF records with site files to verify that investigators were always using the latest safety information. Any discrepancy indicates a failure in document control. To maintain alignment, your process should include:
- Immediate Filing: The final, approved IB should be filed in the eTMF without delay, tagged with clear metadata such as version number, approval date, and effective date.
- Preservation of Past Versions: All older versions of the IB must be retained in the TMF and clearly marked as "superseded" to maintain the historical narrative of the product's evolving safety profile.
- Linking to Distribution Records: The eTMF should also contain distribution logs and investigator acknowledgments, creating a closed-loop audit trail.
Maintaining TMF health is a critical operational function. For a more detailed look at its structure and importance, see our article on the Trial Master File in our detailed guide.
The Domino Effect: What Happens After the TMF
Major IB updates, particularly those related to new safety findings, often initiate a series of subsequent actions. A well-designed document control system anticipates these dependencies and integrates them into the update workflow.
A change in the Reference Safety Information (RSI) section is a common trigger. For example, the addition of a new serious adverse reaction to the IB necessitates corresponding updates to other documents to ensure participant protection and regulatory compliance.
The interconnected nature of clinical trial documentation means a single IB update can initiate a cascade of related changes. Failure to manage follow-on updates to protocols and ICFs can create widespread non-compliance, threatening both participant safety and trial integrity.
This often requires prompt action on several fronts:
- Protocol Amendments: If new risk information alters the trial's risk-benefit balance, a protocol amendment may be necessary to introduce new monitoring procedures, modify eligibility criteria, or adjust study conduct.
- Informed Consent Form (ICF) Revisions: Participants must be informed of any new risks. This requires updating the ICF with the new safety information and subsequently re-consenting all active participants in the study.
This broader perspective underscores the importance of a centralized system. Managing these interconnected updates via email and spreadsheets increases the risk of error. A missed ICF update or a forgotten protocol amendment following an IB change can have serious consequences, reinforcing the need for a systematic approach to investigator’s brochure updates and documentation control.
How Technology Strengthens Your IB Management Process
Managing investigator’s brochure updates and documentation control with manual tools like spreadsheets and email introduces significant compliance risks. Modern clinical documentation platforms can help organizations transition from fragmented, manual processes to a centralized, controlled environment.
These systems provide features designed to support regulatory requirements and enforce operational discipline throughout the IB lifecycle.
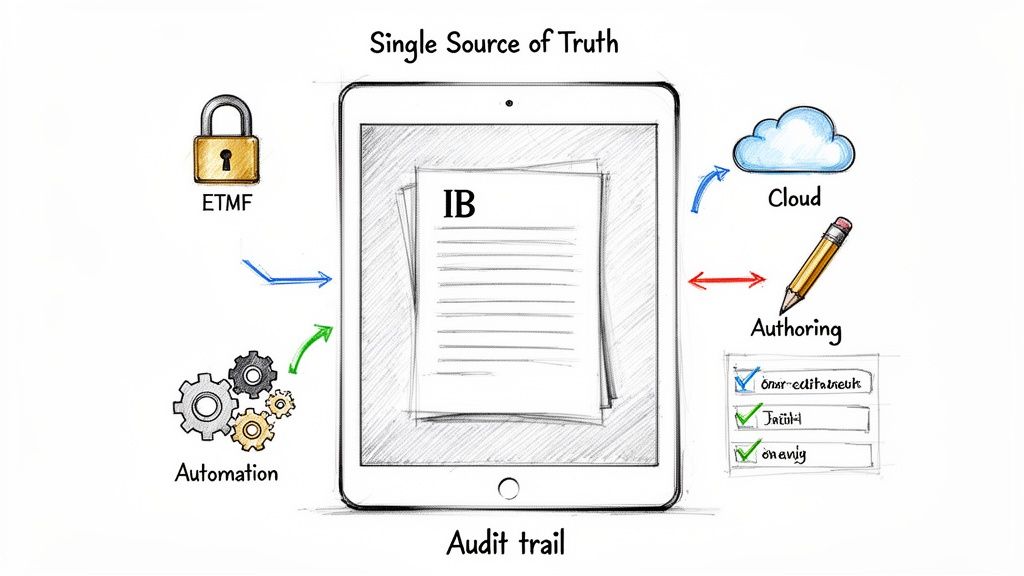
The primary purpose of this technology is to mitigate human error by creating a single source of truth. This ensures that all stakeholders—from medical writers to principal investigators—are working from the most current, correct information. This consistency is fundamental to trial integrity and continuous inspection-readiness.
Starting Strong with Structured Authoring and ICH-Ready Templates
Effective IB management begins at the authoring stage. Purpose-built platforms often include structured authoring tools that offer significant advantages over traditional word-processing software. Users build the IB from pre-approved components and templates aligned with ICH guidelines.
This approach moves away from unstructured documents where copy-paste errors and inconsistencies are common. Content is managed in a controlled, modular fashion. For example, a template can enforce the inclusion of all required ICH E6 sections. When a piece of data, such as a nonclinical study summary, is updated, the change can be propagated across all relevant sections, ensuring consistency is built into the process.
Taming Chaos with Automated Version Control and Audit Trails
Manual versioning is a common source of documentation errors. A dedicated platform automates version control and audit trails, eliminating guesswork.
A purpose-built system functions as an impartial, automated archivist. It captures every touchpoint—every view, comment, edit, and approval—creating an immutable, timestamped audit trail that provides verifiable proof of a controlled process during a regulatory inspection.
This automation includes:
- Automatic Version Numbering: The system assigns clear, sequential version numbers (e.g., v4.0, v4.1), preventing duplicates and confusion.
- Built-in Audit Logs: Every action taken on the document is automatically logged with user and timestamp information, creating a contemporaneous history.
- Controlled State Transitions: The platform manages the document's status—from
DrafttoIn ReviewtoApproved—based on pre-defined workflows, preventing the inadvertent distribution of unapproved versions.
Centralizing Review, Approval, and Distribution
Managing reviews and approvals via email is inefficient and creates a fragmented documentation trail. A centralized platform streamlines this process into a transparent workflow.
Reviewers are automatically notified, and all comments, discussions, and resolutions are captured within the system, creating a single record of decision-making.
Once the IB is approved, the platform can manage distribution to all investigators, sites, and IRBs/IECs. With integrated distribution logs and e-signature capabilities for acknowledgment, a real-time dashboard can show who has received and confirmed review of the new safety information. This closed-loop process provides the concrete evidence of compliance that inspectors require, solidifying the foundation of your investigator’s brochure updates and documentation control.
Thinking Ahead: Future-Proofing Your IB Documentation
Effective management of investigator’s brochure updates and documentation control is fundamental to patient safety and clinical trial integrity. A robust IB management strategy relies on rigorous governance, meticulous change control, clear versioning, and an auditable distribution process. A failure in any of these areas introduces significant risk.
Regulatory expectations are evolving, as evidenced by upcoming guidelines like ICH E6(R3). Regulators increasingly expect structured, traceable, and digitally native documentation. They seek evidence of proactive and systematic lifecycle management, not reactive processes. This necessitates a re-evaluation of manual, spreadsheet-driven workflows that are inherently prone to error.
Shifting from Reactive to Proactive
A forward-looking documentation strategy should be designed for the future. This involves integrating technology into the quality management system to create workflows where compliance is an inherent part of the process, not an additional step.
When this approach is adopted, every version of the IB is inspection-ready, providing a clear and defensible history of the product's evolving safety profile.
A future-proof strategy incorporates several key elements:
- A Single Source of Truth: Centralize all IB-related activities, from drafting to distribution, eliminating the need to search across multiple systems.
- Smart Automation: Utilize technology to manage review cycles, approvals, and distribution, reducing human error and automatically building the audit trail.
- Connected Systems: Ensure the IB management process integrates seamlessly with the eTMF and other regulatory systems to maintain consistency across the organization.
Ultimately, future-proofing your IB strategy involves embedding control and foresight into daily operations. A systematic, technology-enabled approach is no longer just an advantage—it is a necessity for maintaining compliance and protecting the integrity of clinical research.
Frequently Asked Questions
Clinical operations and regulatory teams often encounter practical questions when managing Investigator's Brochure updates. Here are answers to some of the most common inquiries, based on regulatory requirements and operational experience.
How Often Should an Investigator’s Brochure Be Updated?
According to ICH E6(R2), the IB should be reviewed at least annually. However, the guiding principle is that it must be updated whenever significant new information becomes available.
"Significant" new information is data that could alter an investigator's risk assessment. This typically includes:
- New findings from nonclinical studies that change the understanding of the product's safety profile.
- Emerging clinical data, particularly newly identified serious adverse reactions, that affect the risk-benefit analysis.
- Changes in the product's manufacturing or formulation that could potentially impact its safety or pharmacology.
For programs involving high-risk compounds or those with rapidly emerging data, the IB may need to be updated more frequently than once a year. The primary objective is to ensure investigators always have the most current and complete information to protect trial participants.
What Is the Difference Between an IB Amendment and an Addendum?
While the terms are sometimes used interchangeably, an amendment and an addendum serve distinct purposes.
An IB amendment is a full revision of the document. New information is integrated directly into the body of the IB, creating a new, consolidated version (e.g., moving from Version 4.0 to Version 5.0).
An IB addendum is a targeted, supplemental update used to disseminate critical new safety information that cannot wait for the next full amendment. It is a shorter, separate document. A common trigger for an addendum is the identification of a new Suspected Unexpected Serious Adverse Reaction (SUSAR). The addendum is distributed immediately, and the information is later incorporated into a full IB amendment.
Both document types are subject to the same requirements for documentation control, distribution tracking, and site acknowledgment.
Who Is Responsible for Approving Investigator's Brochure Updates?
While the sponsor holds the ultimate responsibility for the IB's accuracy and content, its approval is a collaborative process involving multiple functions with defined roles.
Final approval of an Investigator’s Brochure is a shared responsibility. It requires a formal, documented consensus between medical, safety, and regulatory experts to ensure the document is scientifically sound, clinically relevant, and fully compliant with global standards.
Internal SOPs should clearly define the approval workflow, which typically requires formal sign-off from:
- A qualified medical expert (e.g., a physician) to verify the clinical accuracy and interpretation of the data.
- A representative from pharmacovigilance or product safety to confirm the completeness and correctness of the risk information.
- A specialist from regulatory affairs to ensure the update complies with all relevant global guidelines.