Regulatory inspections are a critical checkpoint in the clinical development lifecycle, serving to verify the integrity of trial data and ensure the protection of participant rights and safety. For professionals in pharmaceutical, biotech, and contract research organizations (CROs), maintaining impeccable documentation is not merely an administrative task. It is the foundation of a successful regulatory submission and a direct reflection of a trial’s operational integrity.
Despite robust quality systems, inspections frequently uncover systemic gaps and inconsistencies that can undermine trial credibility. Understanding the most common documentation findings during regulatory inspections is an essential step toward building proactive quality systems that can withstand regulatory scrutiny. This article provides a detailed overview of ten frequent documentation-related observations, focusing on their root causes and regulatory context.
This overview is designed for experienced clinical operations, quality, and regulatory affairs professionals familiar with clinical trial fundamentals. The focus is on how these findings relate to the lifecycle management and oversight of key documents, from protocols and informed consent forms to statistical analysis plans and clinical study reports. The objective is to provide practical insights that help teams identify and remediate documentation vulnerabilities before they become critical inspection findings.
1. Incomplete or Missing Protocol Deviations Documentation
One of the most frequent findings during regulatory inspections involves the inadequate management of protocol deviations. This issue arises when deviations are not promptly identified, thoroughly documented, consistently tracked, or appropriately justified. The absence of a complete and contemporaneous record undermines the integrity of the clinical trial by creating uncertainty about protocol adherence, subject safety, and the reliability of the collected data.
Inspectors scrutinize deviation logs for completeness, accuracy, and proper authorization. Common gaps include missing investigator signatures, failure to document sponsor review for significant deviations, or vague justifications that do not adequately explain the reason for the departure from the protocol. Such omissions can be interpreted as a systemic failure in trial oversight.
Root Causes and Regulatory Context
These findings often stem from decentralized or manual tracking methods, such as standalone spreadsheets, which are prone to version control issues and incomplete entries. Ambiguous Standard Operating Procedures (SOPs) that fail to clearly define what constitutes a deviation can also lead to inconsistent reporting across sites. From a regulatory perspective, robust deviation management is a cornerstone of Good Clinical Practice (GCP), as it demonstrates that the rights, safety, and well-being of trial subjects are protected and that the trial data are credible. A clear understanding of the differences between deviations and amendments is essential for maintaining compliance. To explore this topic further, you can find more information about the documentation implications of protocol deviations versus protocol amendments.
Systemic Issues and Lifecycle Management
To mitigate these risks, organizations should establish a robust, centralized system for managing protocol deviations. Effective strategies focus on process integrity and include:
- Implementing a Centralized System: Utilize a validated system for real-time deviation reporting, tracking, and review. This ensures all stakeholders work from a single source of truth.
- Defining Clear SOPs: Develop and train staff on clear SOPs that categorize deviations and outline specific reporting and approval workflows for each.
- Standardizing Documentation: Use standardized templates that capture essential information, including a detailed description of the deviation, root cause, corrective actions taken, and impact assessment.
- Conducting Regular Audits: Perform periodic internal audits of deviation logs during monitoring activities to identify and address documentation gaps proactively.
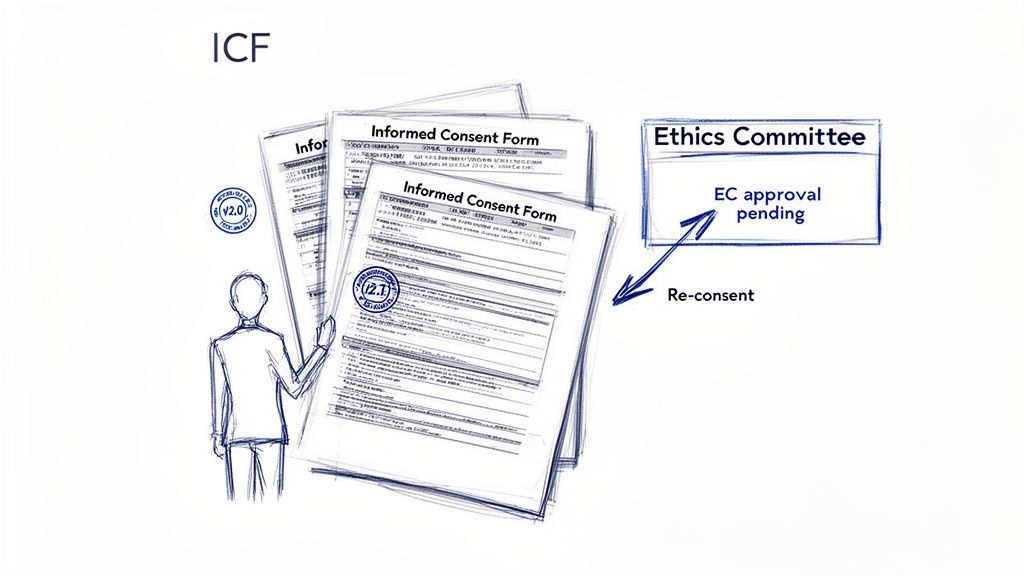
2. Inadequate Informed Consent Form (ICF) Updates and Amendments
Another one of the most common documentation findings during regulatory inspections is the failure to properly manage Informed Consent Form (ICF) updates and amendments. This issue arises when ICFs are not revised, reapproved, and re-consented in a timely manner following protocol amendments or the emergence of new safety information. Deficiencies in version control, Institutional Review Board (IRB) or Ethics Committee (EC) submission, and distribution to sites create significant compliance risks and can compromise participant protection.
Inspectors frequently identify cases where outdated ICF versions remain in use long after an amendment has been approved. Other common findings include failing to secure IRB/EC approval for ICF changes before implementation or not re-consenting participants when new, significant risk information becomes available. Such oversights call into question the validity of the consent process and the sponsor's commitment to participant safety.
Root Causes and Regulatory Context
These documentation gaps often result from disconnected processes where protocol amendments and ICF management are handled in silos. A lack of clear procedures for determining which changes necessitate re-consent can also lead to inconsistent practices across sites. From a regulatory standpoint, the informed consent process is a fundamental tenet of Good Clinical Practice (GCP) and human subject protection. Any failure to keep participants fully informed of relevant new information is a serious breach of ethical and regulatory obligations. To ensure compliance, it is critical to develop a structured approach for managing informed consent updates during ongoing trials.
Systemic Issues and Lifecycle Management
To prevent these findings, organizations must integrate ICF lifecycle management directly into their overall clinical trial oversight framework. Effective strategies include:
- Establishing Integrated Workflows: Create procedures that link protocol amendment approval directly to the ICF revision, IRB/EC submission, and site distribution processes.
- Implementing Robust Version Control: Utilize a centralized repository to manage all ICF versions, ensuring that only the most current, approved version is accessible to clinical sites.
- Defining Re-Consent Criteria: Develop clear, documented criteria for when an ICF change is considered substantive enough to require active re-consent from all affected participants.
- Standardizing Submission Packages: Use standardized templates for ICF amendments and justification documents to ensure consistency and completeness for every IRB/EC submission.
- Tracking Participant Consent: Maintain meticulous records documenting which version of the ICF was signed by each participant and on what date, especially when re-consent occurs.
3. Incomplete or Missing Adverse Event (AE) and Pharmacovigilance Documentation
One of the most critical and frequently cited common documentation findings during regulatory inspections is the failure to maintain complete and accurate records for adverse events (AEs) and pharmacovigilance activities. This issue encompasses deficiencies from missing AE onset dates, severity, and causality assessments to delayed reporting of Serious Adverse Events (SAEs) and inadequate documentation of safety committee oversight. Such gaps compromise the integrity of the product's safety profile.
Inspectors meticulously review AE source documents, case report forms (CRFs), and safety databases to ensure every event is captured, assessed, and reported according to the protocol and regulatory timelines. Common findings include incomplete follow-up on ongoing AEs, inconsistent seriousness classifications between the site and sponsor, or missing documentation of timely submission of expedited reports to regulatory authorities. These omissions can suggest a systemic breakdown in an organization's safety monitoring and reporting obligations.
Root Causes and Regulatory Context
These documentation gaps often arise from inconsistent data collection practices across sites, a lack of clear guidance on causality assessment, and manual tracking systems that fail to provide visibility into reporting deadlines. Ambiguous processes for reconciling safety databases with clinical databases can also lead to discrepancies. From a regulatory standpoint, comprehensive AE documentation is fundamental to Good Pharmacovigilance Practices (GVP) and GCP, as it forms the basis for characterizing a product’s safety profile and protecting trial participants.
Systemic Issues and Lifecycle Management
To fortify safety documentation and reporting, organizations must implement robust and standardized pharmacovigilance systems. Effective strategies include:
- Standardizing Data Collection: Implement standardized AE collection forms in the Electronic Data Capture (EDC) system with required fields to ensure all critical data points are captured at the source.
- Establishing Clear Procedures: Develop clear SOPs and provide comprehensive training to investigators on AE grading, causality assessment, and reporting timelines aligned with ICH guidelines.
- Automating Safety Workflows: Utilize a centralized safety reporting system with tracking of reporting deadlines for SAEs and other expedited reports, triggering alerts to prevent late submissions.
- Implementing Centralized Review: Establish a formal medical review process where all AEs are assessed for causality and seriousness in a consistent, documented manner.
- Maintaining Comprehensive Files: Create and maintain thorough pharmacovigilance files containing safety reports, regulatory correspondence, and safety committee meeting minutes to provide a complete audit trail of safety oversight.
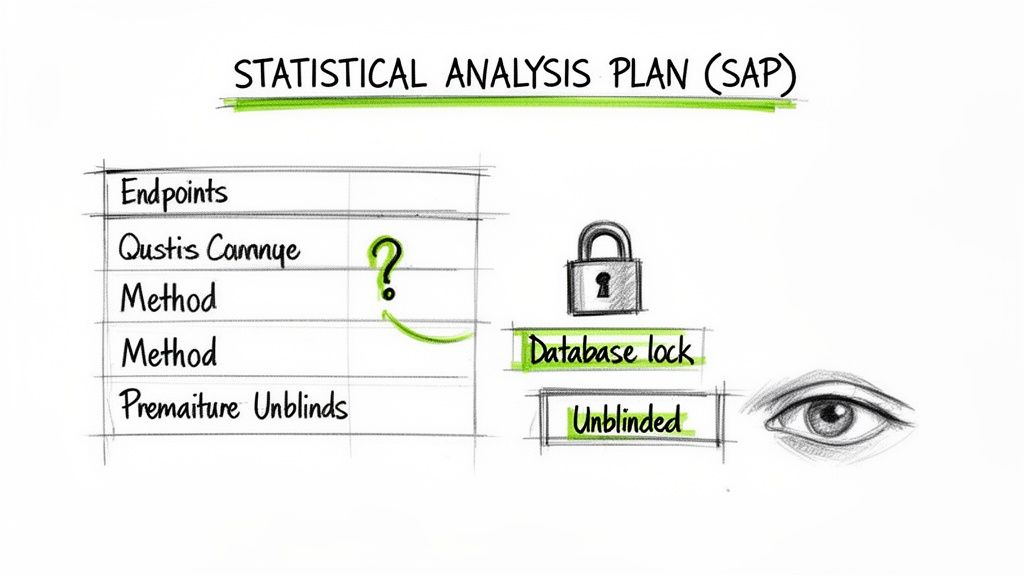
4. Deficient Statistical Analysis Plan (SAP) Documentation and Deviations
Another frequent source of findings during regulatory inspections is a deficient Statistical Analysis Plan (SAP). This issue manifests as SAPs that lack sufficient detail, are not finalized in a timely manner, or fail to document deviations from the pre-specified analyses. Such deficiencies compromise the scientific validity of the trial results by introducing the potential for bias in the analysis and interpretation of the data.
Inspectors review the SAP to ensure it prospectively defines the statistical methods for analyzing the trial data. Common gaps include vague endpoint definitions, failure to pre-specify methods for handling missing data, and evidence that the SAP was finalized after database lock or unblinding. These issues call into question whether the analyses were truly pre-specified or were influenced by the observed data.
Root Causes and Regulatory Context
These deficiencies often originate from a lack of cross-functional collaboration early in the trial, delaying the development and finalization of the SAP. Inadequate version control and a poorly defined finalization process can lead to the plan being signed off after key milestones. Per ICH E9 (Statistical Principles for Clinical Trials), the SAP should be finalized before the treatment blind is broken. Failure to do so can lead regulators to question the objectivity of the statistical analyses and the credibility of the study's conclusions. You can explore best practices by reading more about Statistical Analysis Plan lifecycle management.
Systemic Issues and Lifecycle Management
To prevent these findings, organizations must treat the SAP as a critical, controlled document with a defined lifecycle. Effective strategies include:
- Establishing Clear Timelines: Define and enforce a timeline that requires the SAP to be finalized and signed before any unblinding of data or database lock.
- Developing Standardized Templates: Use a robust, standardized SAP template aligned with ICH E3 and E9 that mandates detailed specifications for all analysis populations, endpoints, and statistical methods.
- Implementing Blind Data Review: Institute a formal blind data review process where the statistical team can review the "clean" data for programming and quality checks while remaining blinded to treatment allocation until the SAP is locked.
- Documenting All Changes: Maintain a clear audit trail of the SAP's development, including version history, review comments, and final approvals, to demonstrate its prospective nature.
- Formalizing Deviation Management: Create a formal process for documenting any deviations from the finalized SAP, including a scientific justification and an assessment of their impact on the study results, within the Clinical Study Report (CSR).
5. Inadequate Quality Overall Summary (QOS) or Chemistry and Manufacturing Controls (CMC) Documentation
A significant number of regulatory submission delays and inspection findings trace back to insufficient or poorly organized Chemistry and Manufacturing Controls (CMC) documentation. These issues often manifest as gaps in the Quality Overall Summary (QOS), where critical data on drug substance, drug product, and manufacturing processes are either missing, contradictory, or inadequately justified. Inspectors review this documentation to ensure product quality, consistency, and safety.
Common deficiencies include incomplete analytical method validation reports, missing batch analysis data for pivotal lots, or stability protocols that do not align with ICH guidelines. For example, a submission may be delayed if the CMC documentation lacks sufficient detail on manufacturing process validation. Such findings indicate a potential breakdown in the quality management system.
Root Causes and Regulatory Context
These documentation gaps often originate from a disconnect between early-stage development activities and late-stage regulatory submission requirements. A failure to establish a robust quality strategy aligned with ICH Q8, Q9, and Q10 principles early on can result in a disjointed and incomplete data package. The lack of standardized templates and clear version control for master quality documents further exacerbates the problem.
From a regulatory standpoint, comprehensive CMC documentation is essential. It provides the evidence that a manufacturer can consistently produce a product of intended quality. Inadequate documentation not only undermines the credibility of the submission but also raises questions about the sponsor's ability to maintain control over their manufacturing processes, a key focus during inspections.
Systemic Issues and Lifecycle Management
To prevent these common documentation findings during regulatory inspections, organizations must implement proactive quality and documentation management strategies. Effective plans include:
- Establishing a Quality Master Plan: Develop a comprehensive quality plan early in the product lifecycle that aligns with ICH guidelines and outlines all required CMC documentation for each development phase.
- Standardizing Document Templates: Create and enforce the use of standardized templates for all CMC-related documents, including batch records, validation plans, and stability reports, to ensure consistency.
- Developing Comprehensive Validation Plans: Author detailed analytical method and process validation plans with predefined acceptance criteria before initiating pivotal studies.
- Maintaining Traceable Batch Records: Ensure all batch records are meticulously detailed, documenting in-process controls, deviations, and justifications for any out-of-specification results.
- Conducting Pre-Submission Gap Analyses: Perform a thorough internal audit or gap analysis of the QOS and all supporting CMC documentation against regulatory requirements well before the planned submission date.
6. Inadequate Clinical Trial Agreement (CTA) and Study-Specific Documentation
A fundamental yet common area for regulatory scrutiny is the documentation surrounding Clinical Trial Agreements (CTAs) and other essential study-specific agreements. Findings in this category often involve CTAs that are missing, incompletely executed, or lack clear definitions of investigator responsibilities. Such issues compromise the legal and regulatory foundation of the trial, raising questions about investigator accountability and site authorization to conduct the study.
Inspectors review these contractual documents to verify that a formal, legally binding agreement was in place before any trial activities commenced. Gaps, such as absent signatures from all required parties, missing financial disclosures, or budget documentation that does not align with the protocol, can lead to significant findings. For example, a trial may be found to have initiated activities at sites lacking fully executed CTAs, a critical oversight that questions the validity of site operations from the outset.
Root Causes and Regulatory Context
These documentation gaps often arise from a lack of centralized oversight and standardized templates for site agreements. When individual sites or regions create bespoke contracts without harmonized legal and regulatory input, inconsistencies and omissions are more likely. The absence of a robust tracking system to monitor agreement execution status across all sites can also lead to studies starting without proper authorization. From a regulatory standpoint, the CTA is a cornerstone document that formalizes the investigator's commitment to adhering to GCP, protocol requirements, and applicable regulations. Incomplete or missing agreements undermine this commitment.
Systemic Issues and Lifecycle Management
To prevent these common documentation findings during regulatory inspections, organizations must implement stringent controls over trial agreements. Effective strategies include:
- Developing Standardized Templates: Create and mandate the use of a master CTA template that has undergone thorough legal and regulatory review. This ensures all essential clauses are included consistently.
- Establishing Pre-Enrollment Execution Mandates: Implement a policy that prohibits participant enrollment at any site until the CTA and all associated agreements are fully executed by all parties.
- Implementing Systematic Tracking: Use a centralized system or tracker to monitor the status of all site agreements from draft to final execution.
- Defining Comprehensive Terms: Ensure agreements clearly delineate all investigator obligations, data ownership, financial terms, and responsibilities for regulatory reporting.
- Integrating Compliance Checks: Incorporate a formal check of CTA and agreement status into the site initiation visit (SIV) checklist, ensuring documentation is complete before activating the site.
7. Incomplete or Inadequate Investigator's Brochure (IB) Documentation and Updates
Another one of the most common documentation findings during regulatory inspections centers on the Investigator’s Brochure (IB). Inspectors frequently identify IBs that are outdated, incomplete, or lack a documented history of review and distribution. This document serves as the single source of truth for investigators regarding the investigational product's nonclinical and clinical data. Failures to maintain its accuracy and completeness can directly impact subject safety.
Inspectors review the IB to ensure it reflects the most current safety and efficacy information available to the sponsor. Common deficiencies include the failure to incorporate emerging safety signals from ongoing trials, missing sections required by ICH E6, or a lack of version control that demonstrates timely updates and approvals. For example, an inspection might identify an IB that was not updated after new safety data emerged, representing a significant gap in communicating risk to investigators.
Root Causes and Regulatory Context
These documentation gaps often arise from a lack of a systematic process for monitoring new data, such as published literature or findings from other studies. Without a formal, scheduled review cycle, IB updates can become an ad-hoc activity that is easily overlooked. From a regulatory standpoint, the IB is a foundational component of Good Clinical Practice (GCP). It ensures that investigators have the necessary information to conduct the trial safely and ethically. An inadequate IB suggests a failure in the sponsor's responsibility to keep investigators fully informed.
Systemic Issues and Lifecycle Management
To prevent these findings, sponsors should implement a structured lifecycle management process for the IB. Effective strategies include:
- Establishing Systematic Monitoring: Implement a documented process for systematic literature and safety database reviews to proactively identify new information relevant to the investigational product.
- Scheduling Periodic Reviews: Mandate periodic IB reviews, at a minimum annually, and trigger ad-hoc updates whenever significant new safety information emerges. This process should be defined in an SOP.
- Maintaining Version Control and Distribution Logs: Implement robust version control for all IB updates, including documented approvals from a cross-functional team. A comprehensive distribution log is essential to confirm that all investigators have received and acknowledged the current version.
- Using Standardized Templates: Develop and use a standardized IB template that is fully aligned with ICH E6 guidance, ensuring all required sections are present and consistently populated.
- Integrating IB Review into Monitoring: Include a review of IB receipt and investigator acknowledgment as a standard component of site monitoring and internal audit procedures to verify compliance at the site level.
8. Missing or Deficient Study Site Audit and Inspection Documentation
Inadequate documentation related to oversight activities, such as monitoring visits and site audits, represents a significant gap frequently cited during inspections. This finding encompasses a range of issues, from missing monitoring visit reports and incomplete follow-up on action items to insufficient records of investigator training. A deficient audit trail for oversight activities calls into question the sponsor's ability to ensure trial integrity, subject safety, and data quality across participating sites.
Inspectors review monitoring reports, audit certificates, and related correspondence to verify that the sponsor is actively overseeing trial conduct. Common deficiencies include reports that lack detail on source document verification (SDV), failure to document that issues identified in previous visits were resolved, or an absence of records confirming that site staff received necessary protocol and GCP training. These omissions can suggest a systemic breakdown in the sponsor's quality management system.
Root Causes and Regulatory Context
These documentation gaps often arise from inconsistent reporting practices across monitors, the use of non-standardized templates, and a lack of a centralized repository for oversight records. When monitoring documentation is stored in disparate locations, it becomes difficult to demonstrate a complete and contemporaneous oversight history. From a regulatory standpoint, ICH-GCP Section 5.18.4 mandates that sponsors ensure monitors are appropriately trained and that monitoring activities are thoroughly documented. Failure to do so undermines the credibility of the sponsor's oversight responsibilities.
Systemic Issues and Lifecycle Management
To fortify oversight documentation, organizations must standardize and centralize their monitoring and audit processes. Effective strategies include:
- Standardizing Report Templates: Develop and implement comprehensive, standardized templates for monitoring visit reports that mandate the inclusion of key elements like SDV scope, findings, action items, and resolution status.
- Establishing Centralized Repositories: Use a validated system, such as an eTMF, to serve as a single, access-controlled repository for all monitoring reports, follow-up correspondence, and audit documentation.
- Implementing Formal Follow-Up Procedures: Create and enforce SOPs that require documented follow-up on all identified issues, including verification that corrective actions have been implemented effectively.
- Maintaining Comprehensive Training Logs: Keep detailed and current training records for all site personnel, including signed attendance sheets and certificates for protocol, GCP, and other relevant training.
- Documenting the Monitoring Plan: Develop a formal monitoring plan prior to trial initiation that clearly outlines the scope, methods, and frequency of monitoring activities, and ensure it is followed and documented.
9. Deficient Clinical Study Report (CSR) Documentation and Completeness
A Clinical Study Report (CSR) that is incomplete or inadequately documented is a major issue during regulatory inspections. This finding arises when the final report fails to provide a comprehensive, unambiguous description of the study's conduct and results, as outlined in ICH E3 guidance. Issues often include missing details on methodology, incomplete analyses, or conclusions that are not fully supported by the underlying data.
Inspectors review CSRs to ensure they accurately reflect the study's execution and provide a complete picture of its efficacy and safety outcomes. Common deficiencies include inadequate discussion of safety signals, discrepancies between the CSR and source data, and insufficient justification for statistical methods. These gaps compromise the report's integrity and can lead to questions about the validity of the study’s conclusions.
Root Causes and Regulatory Context
Deficiencies in CSRs often originate from a lack of a structured development plan and insufficient quality control. Without a standardized template and a clear writing plan established early in the trial, teams may struggle to ensure all required sections are addressed consistently and thoroughly. Inadequate cross-functional review involving biostatistics, medical, and regulatory experts can also lead to critical omissions.
From a regulatory standpoint, the CSR is a cornerstone of a marketing application, and its completeness is essential. An inadequate CSR can result in submission delays or requests for additional information. These common documentation findings during regulatory inspections signal a failure in the sponsor's quality management system and its ability to produce a reliable account of the clinical trial.
Systemic Issues and Lifecycle Management
To prevent CSR-related findings, organizations must implement a rigorous, proactive approach to its development and review. Effective strategies include:
- Establishing a CSR Writing Plan: Develop a comprehensive plan early in the study lifecycle that aligns with ICH E3 and outlines timelines, roles, and responsibilities for each section.
- Using Standardized Templates: Create and enforce the use of a standardized CSR template that includes all required sections and subsections, ensuring consistency across all studies.
- Implementing Robust Quality Control: Institute a multi-stage quality assurance process that includes independent review of data, verification of conclusions against source documentation, and thorough medical review of safety interpretations.
- Mandating Cross-Functional Sign-Off: Establish a formal sign-off procedure requiring review and approval from key functional areas, including biostatistics, clinical operations, medical, and regulatory affairs, before finalization.
- Maintaining Clear Audit Trails: Ensure any amendments or corrections to the CSR are formally documented, justified, and version-controlled to maintain a clear and traceable history of the document.
10. Inadequate Documentation of Regulatory Authority Communications and Submissions
A critical finding during regulatory inspections is the failure to maintain a complete and auditable record of all interactions with regulatory authorities. This deficiency includes missing copies of submissions, undocumented feedback, absent meeting minutes, and poor tracking of commitments made to agencies. A disorganized or incomplete history of regulatory correspondence creates risk, as it can lead to missed deadlines, inconsistent responses, and an inability to demonstrate a clear and compliant communication trail.
Inspectors expect a meticulously organized and accessible repository of all formal communications. Gaps such as a missing response to a Request for Information (RFI), or a failure to document commitments made during a Scientific Advice meeting, suggest a lack of procedural control. These omissions can impede an inspector's ability to verify that the sponsor has addressed all agency concerns and complied with regulatory directives.
Root Causes and Regulatory Context
These documentation gaps often arise from a lack of centralized management, with correspondence and submission records scattered across individual email inboxes or local drives. Without standardized procedures for filing, logging, and tracking these critical documents, information is easily lost or overlooked. From a regulatory standpoint, maintaining this correspondence is a fundamental component of demonstrating control and transparency. It provides a historical account of the dialogue with health authorities, substantiating the rationale behind key development decisions.
Systemic Issues and Lifecycle Management
To prevent such common documentation findings, organizations must establish a systematic approach to managing regulatory communications. Effective strategies include:
- Establishing a Centralized Repository: Implement a validated, access-controlled system to serve as the single source of truth for all regulatory submissions, correspondence, and meeting minutes.
- Standardizing Meeting Documentation: Use standardized templates for regulatory meeting minutes that clearly capture attendees, agenda items, key discussions, decisions made, and explicit action items with assigned owners and due dates.
- Implementing a Tracking System: Create a comprehensive log or tracking system that documents every submission, its receipt date, agency feedback, response timelines, and final resolution.
- Developing Clear Procedures: Author and implement SOPs that define the process for receiving, logging, filing, and responding to all regulatory correspondence to ensure consistency.
- Conducting Regular Internal Audits: Perform periodic audits of the regulatory files to proactively identify and correct any gaps in documentation, ensuring the records are inspection-ready at all times.
10-Point Comparison: Common Regulatory Inspection Documentation Findings
| Item | Implementation complexity | Resource requirements | Expected outcomes | Ideal use cases | Key advantages |
|---|---|---|---|---|---|
| Incomplete or Missing Protocol Deviations Documentation | Moderate — establish SOPs and tracking systems | Moderate — e-log, training, monitoring time | Improved traceability and protocol adherence | Ongoing multicenter trials with frequent deviations | Enhanced compliance visibility and inspection readiness |
| Inadequate Informed Consent Form (ICF) Updates and Amendments | Moderate — lifecycle controls and re‑consent workflows | Moderate–High — ethics/IRB coordination, participant contact | Current consent, better participant protection, fewer ethics findings | Trials with safety signals or protocol amendments | Protects participant rights and reduces liability risk |
| Incomplete or Missing AE and Pharmacovigilance Documentation | High — PV systems, expedited reporting workflows | High — PV staff, medical review, safety committees | Robust safety monitoring and timely regulatory reporting | Safety‑critical studies, novel therapies, large multisite trials | Accurate safety profile supporting regulatory decisions |
| Deficient Statistical Analysis Plan (SAP) Documentation and Deviations | Moderate–High — early biostatistics input and version control | Moderate — biostatisticians, documentation governance | Analytical transparency, reduced bias, smoother reviews | Pivotal trials and studies with complex endpoints | Pre‑specification improves reproducibility and credibility |
| Inadequate Quality Overall Summary (QOS) or CMC Documentation | High — validation, stability, supply‑chain documentation | Very high — labs, manufacturing, quality experts | Demonstrated product quality and fewer CMC queries | Biologics, complex drug products, regulatory submissions | Strengthens regulatory confidence in product quality |
| Inadequate Clinical Trial Agreement (CTA) and Study‑Specific Documentation | Low–Moderate — templates and signature workflows | Moderate — legal review, site coordination, tracking | Clear responsibilities, fewer contractual issues | Multi‑site, sponsor‑funded studies | Reduces governance risk and clarifies obligations |
| Incomplete or Inadequate Investigator's Brochure (IB) Documentation and Updates | Moderate — literature monitoring and periodic updates | Moderate — medical writing, safety review, distribution tracking | Up‑to‑date investigator knowledge and safer conduct | Early‑phase studies or rapidly evolving safety data | Ensures investigators have current safety/efficacy information |
| Missing or Deficient Study Site Audit and Inspection Documentation | Moderate — standardized monitoring and audit templates | Moderate–High — monitors, QA, electronic records | Improved oversight, corrective action verification, inspection readiness | Large multisite trials or high‑risk sites | Demonstrates active oversight and quality assurance |
| Deficient Clinical Study Report (CSR) Documentation and Completeness | Moderate–High — cross‑functional synthesis and QA | High — biostatistics, medical writers, QA reviewers | Complete, submission‑ready study report with fewer queries | Pivotal trials and regulatory submissions | Clear presentation of results supporting regulatory decisions |
| Inadequate Documentation of Regulatory Authority Communications and Submissions | Low–Moderate — centralized filing and meeting templates | Moderate — regulatory affairs staff and tracking tools | Clear audit trail, accountable follow‑up, reduced delays | Ongoing regulatory interactions and submission management | Ensures commitments tracked and improves strategy continuity |
Building a Foundation of Proactive Documentation Quality
As the top ten common documentation findings during regulatory inspections demonstrate, these issues are rarely the result of a single oversight. Instead, they are often symptoms of deeper, systemic gaps in documentation lifecycle management and operational oversight.
The findings detailed in this article—inadequate ICF version control, missing pharmacovigilance records, and poorly documented regulatory communications—all point toward a reactive, fragmented approach to clinical documentation. When teams operate in silos using disparate systems and manual processes, consistency and oversight become challenging. This creates vulnerabilities that can be revealed under the scrutiny of an inspector. The core challenge is not just correcting individual documents but re-engineering the foundational processes that create and manage them.
Shifting from Reactive Correction to Proactive Compliance
The most significant takeaway is the need to shift from a reactive, pre-inspection cleanup mentality to a proactive, quality-by-design strategy. Inspection readiness is not a phase; it is the continuous outcome of well-designed, well-executed, and well-documented processes.
To achieve this, organizations must embed compliance directly into their daily workflows. This requires a change in perspective:
- View Documentation as an Asset: Treat clinical trial documentation not as an administrative burden but as the primary evidence of study integrity, patient safety, and data quality.
- Embrace Lifecycle Management: Every document, from the Investigator's Brochure to the final CSR, has a lifecycle that includes structured authoring, review, approval, version management, and archival.
- Prioritize Process Over Product: A complete final document generated from a chaotic process is an anomaly, not a sign of a robust system. Regulators are increasingly focused on the systems and controls that ensure consistent quality, not just the final output.
Actionable Steps Toward Inspection Readiness
Transitioning to a proactive documentation model involves tangible operational and technological changes. A critical step is to centralize and standardize. Utilizing a unified clinical documentation system, designed with regulatory frameworks like ICH E6(R3) in mind, can provide the necessary controls. Such systems can enforce standardized templates, automate version control, and create auditable workflows for review and approval. This helps remove the human error inherent in manual, email-based processes.
Key Insight: Proactive documentation quality is not about having more meetings or creating more checklists. It's about implementing intelligent systems and streamlined workflows that make compliance an inherent part of the work, not an additional task.
Ultimately, mastering documentation is about more than passing an inspection. It is about building a foundation of trust with regulators, partners, and the patients who participate in clinical trials. The common documentation findings during regulatory inspections serve as a critical roadmap, highlighting the precise areas where processes can be strengthened. By addressing these weak points with systemic solutions, organizations can not only de-risk their regulatory interactions but also enhance operational efficiency and the integrity of their clinical research.