Effective TMF quality control and ongoing oversight is a foundational component of an inspection-ready clinical trial. The objective is not merely to collect documents but to establish and maintain a system that demonstrates the integrity of a trial’s conduct from initiation to final submission. A well-defined quality program provides assurance that trial data is verifiable and that the rights, safety, and well-being of subjects are protected.
Laying the Groundwork for TMF Quality
A TMF quality framework serves as the operational blueprint for a study's documentation. It is a comprehensive system built on documented procedures, which aligns with regulatory expectations, such as those outlined in ICH E6(R3), for active sponsor oversight and data integrity.
Central to this framework are two distinct functions: Quality Control (QC) and Quality Assurance (QA). While often used interchangeably in general contexts, these terms have specific meanings in TMF management.
- Quality Control (QC): Refers to the operational checks performed on TMF content. QC is the routine process of reviewing individual documents after filing to verify that they are complete, legible, and correctly indexed according to established procedures. For example, a QC check confirms the presence of required signatures and dates and verifies the correct document version was filed.
- Quality Assurance (QA): Encompasses the oversight of the quality management system itself. QA activities, such as periodic audits, are designed to confirm that the overall quality process, including QC checks, is functioning as intended and is effective in identifying and mitigating risks.
The Role of Standard Operating Procedures
Standard Operating Procedures (SOPs) are the cornerstone of a TMF quality program. They translate regulatory principles into repeatable, actionable instructions for study teams. Without clear SOPs, processes can become inconsistent and ambiguous across sites, vendors, and internal departments.
Industry data indicates that a high percentage of organizations have a dedicated Quality Control SOP. Well-defined SOPs contribute to audit readiness by standardizing workflows, which allows resources to be focused on high-risk areas without compromising overall compliance.
Regulatory inspectors expect to see evidence of a controlled process for managing trial documentation. SOPs provide primary evidence of a systematic approach to quality that was established before study activities commenced.
Core Components of TMF SOPs
An effective SOP should provide clear, unambiguous guidance to ensure every team member understands their role and responsibilities. Our guide on a RACI model for clinical trial documentation can assist in defining these roles.
At a minimum, TMF SOPs should clearly outline:
- Document Handling and Indexing: Procedures for how documents are received, processed, and filed according to the TMF Reference Model, including specifications for metadata, naming conventions, and version control.
- QC Sampling Strategy: The methodology for quality checks, specifying which documents require 100% review and which are subject to a risk-based sampling model.
- Issue Remediation Process: A defined workflow for documenting, tracking, and resolving findings from QC reviews. This should include timelines for correction and a process for root cause analysis to prevent recurrence of issues.
Inspection findings from regulatory authorities such as the FDA and EMA frequently cite TMF disorganization, missing documents, and lack of oversight. These issues can often be traced back to the absence of clear, well-implemented SOPs, highlighting the direct link between procedural documentation and regulatory compliance.
To further clarify, the essential pillars of a robust TMF quality program can be structured as follows.
Core Components of a TMF Quality Framework
| Component | Purpose | Key Activities |
|---|---|---|
| SOPs & Checklists | To create consistent, repeatable processes for TMF management and QC. | Developing, reviewing, and updating SOPs; creating document-specific QC checklists. |
| Roles & Responsibilities | To ensure clear accountability for all TMF-related tasks. | Defining roles using a RACI model; assigning specific QC and oversight duties. |
| QC & Review Schedule | To establish a proactive, risk-based timeline for quality checks. | Setting QC frequency (e.g., within 5 days of upload); defining sampling strategies. |
| Issue Remediation | To systematically track, resolve, and prevent TMF discrepancies. | Logging findings; conducting root cause analysis; implementing corrective actions. |
| Metrics & Reporting | To provide ongoing visibility into TMF health and inspection readiness. | Tracking KPIs (e.g., completeness, timeliness); creating TMF health dashboards. |
| Training & Documentation | To ensure the entire team is competent and aligned on TMF processes. | Conducting SOP training; documenting training records for all team members. |
This table illustrates how each component integrates to form a cohesive, defensible system. When these components function in harmony, TMF management shifts from a reactive process to a proactive state of continuous inspection readiness.
Designing a Practical TMF Quality Control Process
Transitioning from a high-level framework to an operational TMF quality control process requires careful planning. A robust QC process must be tailored to the specific risks and complexities of a clinical trial. The objective is to create a system that withstands regulatory scrutiny without impeding daily operations.
The process begins with the development of comprehensive QC checklists aligned with the TMF Reference Model and internal SOPs. A well-designed checklist provides reviewers with specific, objective criteria against which each document is measured.
For an Informed Consent Form (ICF), a basic checklist might only confirm its presence. A more detailed checklist would prompt the reviewer to verify:
- The protocol and site numbers match trial records.
- The version is the one approved by the IRB for the participant's enrollment date.
- All required signatures and dates are present, legible, and correctly placed.
- No unapproved abbreviations were used.
This level of detail promotes a consistent, evidence-based quality check, independent of the individual reviewer.
This visual represents the process flow. SOPs form the foundation, the QC process comprises the daily operational tasks, and the overarching Quality Assurance program validates the system's effectiveness.
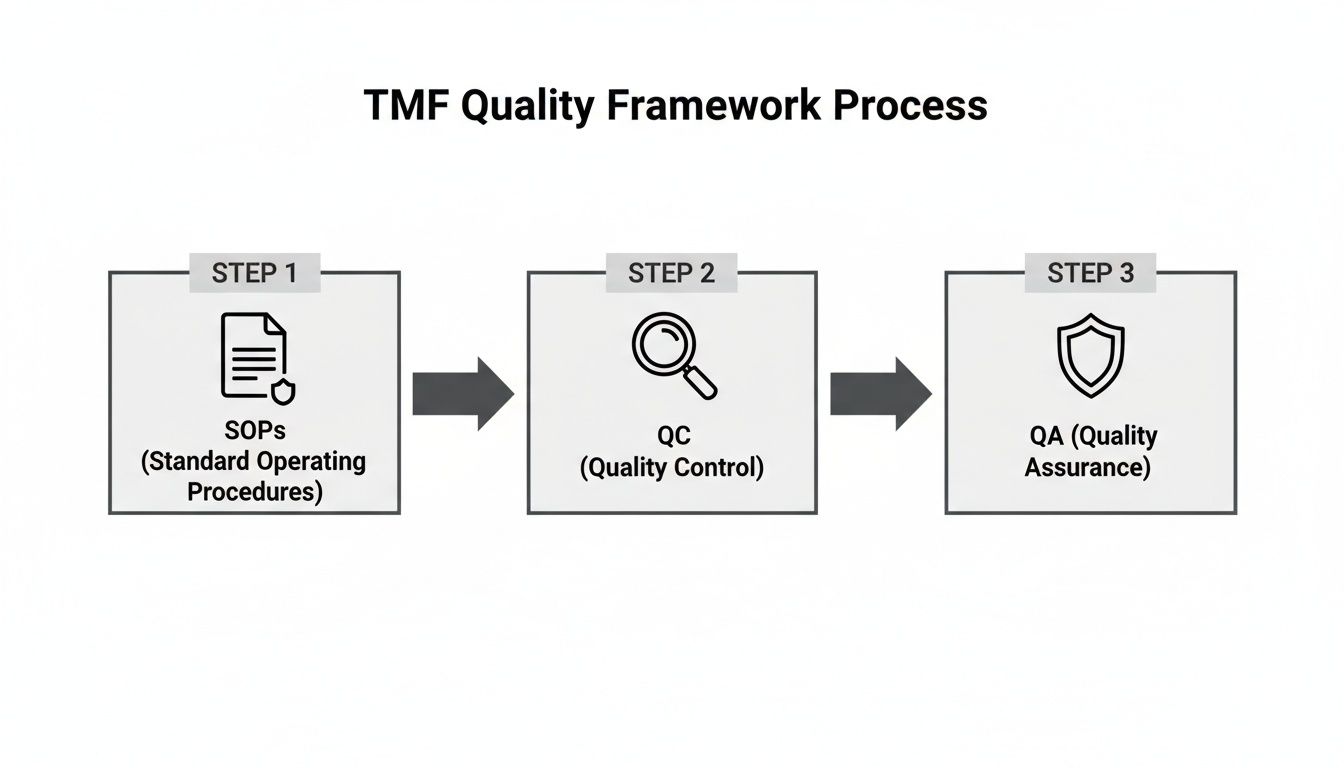
As shown, QC is a central component of a compliant TMF management system, built upon the strategic foundation of standard operating procedures.
Defining Your Sampling Strategy
After establishing checklists, the next step is to define the scope of the review. Performing a 100% QC review on every document is often not feasible or necessary. A risk-based approach allows for the concentration of resources on documents critical to patient safety and data integrity.
A common approach involves categorizing documents by impact:
- High-Impact Documents: These include documents such as Informed Consent Forms, protocol signature pages, and significant safety reports, where an error could have serious consequences. For these artifacts, a 100% QC review is a widely adopted standard.
- Lower-Impact Documents: This category includes items like internal meeting minutes or routine site correspondence. While their presence in the TMF is required, an isolated error is less likely to compromise the trial. For these, a risk-based sampling model, such as reviewing a 10-20% sample periodically, is a common strategy.
This blended approach enables tight control over critical documents while maintaining a manageable workload for other content.
Establishing the Right Timing for QC
The timing of QC checks is as critical as the methodology. Deferring quality control to the end of a study can result in an unmanageable volume of documents and the late discovery of significant errors.
A proactive schedule is preferable. Two common models are:
- Contemporaneous Review: This approach involves performing QC as documents are filed, typically within a predefined window, such as 3-5 business days of upload. This provides real-time feedback to teams and helps maintain the TMF in a state of inspection readiness.
- Periodic Batch Review: This model involves conducting QC on a regular schedule, such as weekly or bi-weekly. While not real-time, it remains proactive and prevents the accumulation of large backlogs, offering a manageable workflow for teams with variable submission volumes.
The rationale is straightforward: the earlier a problem is identified, the less resource-intensive it is to correct. A contemporaneous review process is a best practice for maintaining a constant state of audit readiness.
Assigning Clear Roles and Responsibilities
An effective QC process depends on clearly defined roles and accountability. Ambiguity in responsibilities can lead to missed tasks and a lack of ownership.
A responsibility matrix, such as a RACI chart, can eliminate confusion.
| Task | Responsible Role |
|---|---|
| Document Upload | Clinical Research Associate (CRA) |
| Initial QC Review | TMF Specialist / Document Manager |
| Issue Resolution | Original Document Owner (e.g., CRA) |
| Final QC Verification | Senior TMF Specialist / TMF Lead |
Defining these roles in the TMF Plan and SOPs integrates accountability into the system. Each team member understands their specific responsibilities, ensuring the process operates smoothly from document creation to archival.
Putting Risk-Based TMF Oversight into Practice
Not all documents in a Trial Master File carry the same level of risk. A risk-based approach aligns with the principles of ICH E6(R3) by focusing resources on documents most critical to patient safety and data integrity. This strategic shift moves TMF management from a volume-based task to an intelligent, targeted process of TMF quality control and ongoing oversight.
The process begins with a TMF risk assessment, which should be a dynamic evaluation revisited throughout the study, particularly at major milestones. The objective is to identify which documents and processes are essential for demonstrating trial integrity to regulatory authorities.
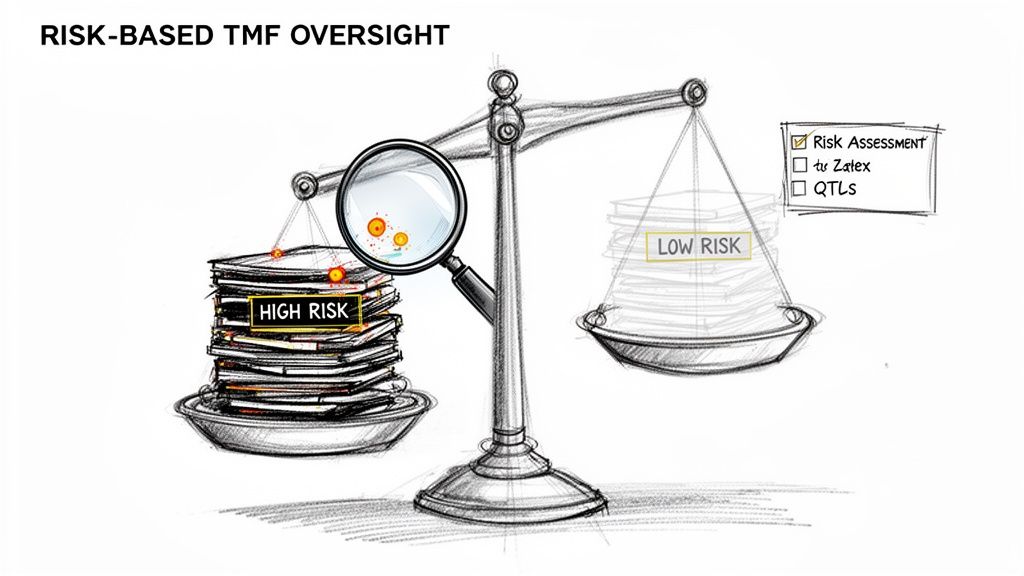
This assessment helps categorize TMF artifacts based on their impact. For example, a missing signature on an informed consent form is a high-risk finding, whereas a typographical error in internal meeting minutes presents a lower risk.
Zeroing In on High-Risk Zones
The first practical step is to identify "high-risk zones"—areas where failures can have a significant negative impact on the trial.
Based on regulatory focus and operational impact, these areas are consistently categorized as high-risk:
- Informed Consent Forms (ICFs): Directly related to patient rights and safety.
- Protocol and Amendments: The foundational document for trial conduct.
- Investigator's Brochure (IB): Contains critical safety information for investigators.
- Safety Reporting Documentation: Essential for pharmacovigilance and subject safety.
- Key Vendor Oversight Documents: Includes contracts and qualification records that demonstrate control over outsourced activities.
By dedicating a higher proportion of QC resources to these zones—often applying a 100% review rate—organizations can strengthen their compliance posture where it is most critical.
Defining Your Quality Tolerance Limits
After identifying high-risk areas, the next step is to define acceptable quality thresholds. Quality Tolerance Limits (QTLs) are predefined thresholds for errors that, if exceeded, may indicate a potential compromise to trial data or patient safety. They provide a measurable definition of "quality."
For example, a team might establish a QTL that no more than 2% of reviewed ICFs can have a missing date. If a monthly QC review identifies a 4% error rate, this would trigger a predefined response, such as retraining site staff or conducting a more intensive review of all ICFs from that site.
QTLs are not intended to achieve perfection but to define an acceptable level of quality and provide a clear, data-driven signal for when intervention is necessary.
Industry groups have explored benchmarks suggesting that a TMF is in a state of good health if deficiencies in high-risk areas remain below a 5% rate.
Moving from Random Sampling to a Targeted Strategy
With a risk assessment and defined QTLs, a QC sampling strategy can be more systematic than a generic "review 10% of everything" approach.
A tiered sampling plan might be structured as follows:
- 100% QC: For documents in high-risk zones, such as ICFs and protocol signature pages.
- 20% random sampling: For medium-risk documents, like site training records or monitoring visit reports.
- 5% periodic spot-check: For low-risk items, such as routine internal correspondence.
This tiered approach ensures that scrutiny is applied where it is most needed, making the overall QC process more efficient and sustainable. Modern electronic trial master file software can be instrumental in automating and tracking these complex, risk-based workflows.
Using Metrics and KPIs for TMF Health Monitoring
Effective TMF management relies on measurement. For TMF quality control and ongoing oversight, subjective assessments are insufficient for regulatory inspections. Key Performance Indicators (KPIs) transform TMF management into a proactive, data-driven discipline.
Tracking relevant metrics provides a real-time assessment of TMF health, enabling teams to identify trends and potential issues before they become significant problems, thereby maintaining a constant state of inspection readiness.
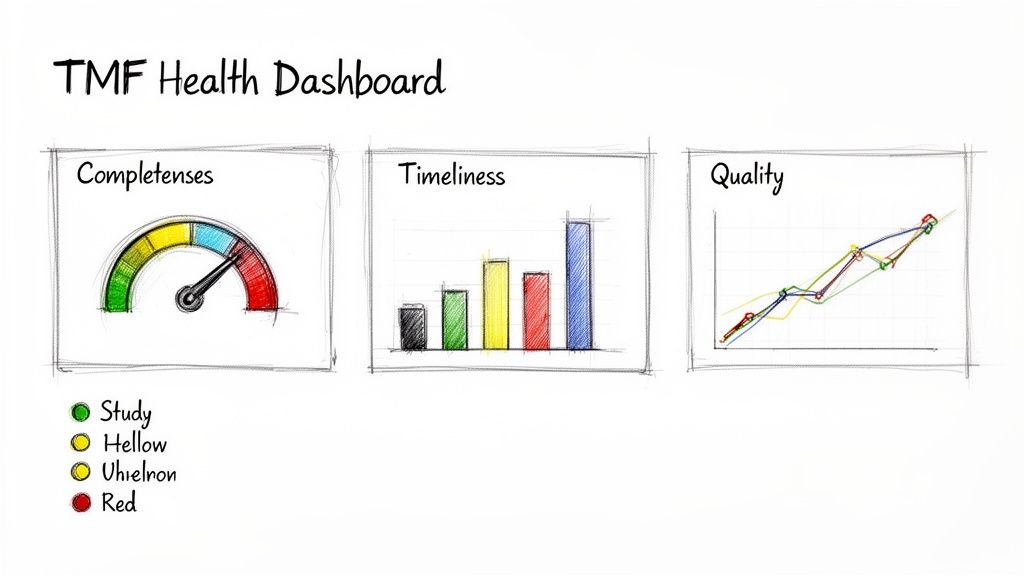
Regulatory inspectors typically evaluate a TMF based on three core principles: completeness, timeliness, and quality. These pillars of TMF health provide a comprehensive view of the trial's documentation status.
Defining Your Core TMF Health Metrics
To build a useful dashboard, it is essential to define what will be measured. Effective KPIs are straightforward to understand, easy to track within an eTMF system, and directly linked to regulatory expectations.
The following foundational metrics are widely considered most important:
- Completeness: The percentage of expected documents that are filed in the TMF. This is calculated by comparing filed documents against the list of expected documents in the TMF Plan for a given milestone.
- Timeliness: The time elapsed between a document's finalization or receipt and its filing in the TMF. A common target is filing within 5-10 business days.
- Quality: The accuracy and acceptability of filed documents. This is often measured as the "first-pass quality rate"—the percentage of documents that pass QC without requiring correction.
These three metrics serve as the vital signs of a TMF. A decline in any of them can signal a breakdown in a process that requires investigation.
For a more detailed examination of a key pillar, refer to our guide on achieving trial master file completeness and inspection readiness.
Essential TMF Health KPIs and Industry Benchmarks
This reference table outlines these critical TMF metrics, their calculation, and targets commonly pursued by inspection-ready organizations.
| KPI | How to Measure | Industry Benchmark |
|---|---|---|
| Completeness | (Actual Documents Filed / Expected Documents) x 100 | >95% for an active study; 100% at study closeout |
| Timeliness | Average number of business days from document finalization to filing | 5-10 business days |
| Quality | (Documents Passing QC on First Review / Total Documents Reviewed) x 100 | >95% first-pass quality rate |
Establishing clear benchmarks provides every team member with a concrete goal, turning abstract concepts like "good quality" into objective, measurable targets.
Building a TMF Health Dashboard
Modern eTMF platforms like Skaldi are designed to facilitate the tracking of these KPIs. The data can be consolidated into a centralized dashboard that provides an at-a-glance view of TMF health across studies, countries, sites, or CRO partners.
An effective dashboard visualizes data to tell a story. For example, completeness might be represented as a gauge approaching 100%, while timeliness could be a bar chart showing average filing days per month. This visual approach allows for rapid comprehension of the TMF's status.
A dashboard is more than a reporting tool; it’s a proactive management instrument. It enables study leads to ask targeted questions like, "Why is Site X consistently lagging in timeliness?" or "What caused the drop in our quality metric last quarter?"
Turning Data into Proactive Management
The value of tracking metrics lies in using the data to drive continuous improvement and mitigate risks. A risk-based TMF management approach may use weighted formulas to assess TMF health. For example, some organizations, as noted in a Veeva TMF trend report, have seen significant increases in starting TMF health scores by implementing a composite score that combines quality, timeliness, and completeness, allowing them to benchmark performance across different compounds and CROs.
This is what proactive oversight entails. When a KPI falls below a predefined threshold, it should trigger a planned response, such as a targeted QC review or a meeting with the responsible team. This data-driven strategy ensures that limited resources are focused where they are most needed, enhancing both efficiency and compliance.
Closing the Loop: From QC Findings to Proactive Remediation
Identifying a discrepancy during a TMF quality check is only the first step. A mature TMF quality control and ongoing oversight program is defined by the actions taken after an issue is identified. The objective is not just to correct errors but to understand their root cause and prevent their recurrence, which is fundamental to achieving a state of continuous audit readiness.
This remediation process closes the loop on quality control, transforming QC findings into actionable intelligence that strengthens the TMF. Without a robust remediation process, the same issues—such as missing signatures, incorrect dates, or misfiled documents—are likely to recur, which can be a significant concern for a regulatory inspector.
A strong remediation workflow creates a clear, documented trail demonstrating that problems were not only identified but also systematically corrected and analyzed.
Building a Structured Remediation Process
Tracking TMF issues via emails or spreadsheets is not a controlled process. A formal, structured process, defined in the TMF Plan or a related SOP, is necessary to ensure accountability and provide a clear audit trail for every finding.
The essential components of a remediation process include:
- Log Everything: Every QC finding, regardless of severity, should be logged in a controlled system, such as a dedicated module in an eTMF or a validated tracking log. The entry must capture document details, a description of the issue, the date of discovery, and the reviewer.
- Assign Clear Ownership: The finding must be assigned to the individual responsible for its resolution—typically the document owner—with a defined deadline.
- Conduct Root Cause Analysis (RCA): For significant or recurring issues, correcting the document is insufficient. It is essential to determine why the error occurred. Potential causes could include training gaps, an unclear SOP, or system limitations. Documenting the root cause is critical for developing effective preventive actions.
- Verify and Close: After a document is corrected and resubmitted, a final QC check is required to verify the resolution. Only then can the finding be formally closed in the tracking system.
Correcting a document error without understanding its origin addresses the symptom but not the underlying cause. Proactive remediation involves looking beyond the immediate issue to address systemic weaknesses, a practice that aligns with inspector expectations.
When You Need a CAPA for TMF Deficiencies
A root cause analysis may uncover a systemic problem that extends beyond a single document. In such cases, a more formal Corrective and Preventive Action (CAPA) plan is warranted. A CAPA is a structured response designed to both fix the immediate problem (corrective action) and implement changes to prevent it from happening again (preventive action).
For example, if QC processes repeatedly find that sites are using an outdated version of a form, a CAPA might include:
- Corrective Action: Identify and replace all incorrect forms in the TMF and notify all affected sites to cease using the obsolete version immediately.
- Preventive Action: Implement a system control that automatically archives outdated templates, retrain all site staff on locating the current version, and update the relevant SOP to clarify the process.
Documenting the entire CAPA process in a quality management system (QMS) demonstrates a mature, responsive quality system that is capable of learning and improving.
Best Practices for Sponsor Oversight of Partners
The sponsor retains ultimate responsibility for the TMF, even when trial activities are outsourced to a CRO or other vendors. Effective oversight is a regulatory requirement.
Sponsor oversight begins with clear communication and documented expectations in the TMF Plan. This document should detail the CRO’s responsibilities, the quality metrics to be tracked, and the frequency and format of TMF reviews.
Regular TMF review meetings between the sponsor and the CRO are essential. These meetings should be data-driven, utilizing KPIs and dashboards from the eTMF (such as those in a platform like Skaldi) to discuss TMF health, review outstanding QC findings, and agree on remediation plans. This collaborative approach fosters alignment and helps prevent minor issues from escalating into significant inspection findings.
Getting Ready for a Successful Inspection
All TMF quality activities are ultimately aimed at ensuring readiness for a regulatory inspection. A state of continuous readiness is far preferable to last-minute remediation efforts.
Periodic mock audits are a valuable tool for preparation. These internal exercises simulate a real inspection, testing a team's ability to navigate the eTMF, articulate the trial's story through its documentation, and retrieve requested documents efficiently. A mock audit can effectively identify process weaknesses and areas where additional team training may be needed.
Training is critical. All personnel who may interact with an inspector—from the TMF lead to the study manager—should be prepared. They should be able to explain the TMF structure, describe the quality control process, and discuss how any identified issues were resolved. This level of preparation can transform an inspection from a high-stress event into an opportunity to demonstrate the integrity of the trial.
Answering Your Top TMF Quality Control Questions
Even with a well-defined TMF oversight plan, practical questions often arise during the course of a trial. The following are some common inquiries from clinical operations and regulatory teams.
What's a "Good" QC Failure Rate for a Mature TMF?
There is no single "magic number" for an acceptable failure rate; it depends on the risk level of the documents being reviewed.
For high-risk documents—such as signed Informed Consent Forms or the protocol signature page—the target failure rate should be as close to 0% as possible. For lower-risk documents, like internal team meeting minutes, a rate in the 2-5% range may be acceptable, provided it falls within the study's established Quality Tolerance Limits (QTLs).
The specific rate is less important than having a documented process for root cause analysis to understand why a failure occurred and a plan for remediation (Corrective and Preventive Actions, or CAPAs). The objective of ongoing oversight is continuous improvement, not merely achieving a static target.
How Do We Manage TMF Quality for Documents from Our Vendors?
As the sponsor, you are ultimately responsible for all TMF content, including documents managed by CROs and other vendors. This responsibility cannot be outsourced. Proactive oversight is essential.
The TMF Plan and vendor contracts should explicitly define:
- Deadlines for document submission.
- Required quality and metadata standards.
- A clear, agreed-upon process for issue resolution and communication.
Conducting independent spot-checks of vendor-submitted documents is a recommended practice. This allows for direct, timely feedback and reinforces accountability. Regular TMF review meetings with partners to discuss KPIs and quality trends are also highly effective.
What’s the Difference Between a TMF Review and TMF Quality Control?
Although often used interchangeably, these are two distinct but related activities. Understanding the difference is key to assigning tasks effectively and gaining a complete picture of TMF health.
TMF Quality Control is a tactical, micro-level activity focused on verifying the correctness of individual documents. A TMF Review, in contrast, is a strategic, macro-level assessment of the entire TMF.
Here is a summary of the differences:
| Aspect | TMF Quality Control (QC) | TMF Review |
|---|---|---|
| Scope | Document-level verification. | Holistic assessment of the TMF. |
| Focus | Verifying specific attributes like signatures, dates, and versions. | Assessing overall health, completeness, trends, and potential risks. |
| Goal | To confirm an individual document is accurate and meets all criteria. | To identify gaps and trends across a study, country, or site. |
| Timing | Performed continuously as documents are received or in frequent batches. | Occurs periodically, such as monthly, quarterly, or at key study milestones. |
In essence, QC involves the routine task of checking individual artifacts for correctness. A TMF review utilizes QC data and other metrics to provide a strategic assessment of the TMF's overall status. One process informs the other, providing a comprehensive view of inspection readiness.