Protocol amendments are a necessary and frequent occurrence in clinical research. When an amendment is made, the change impacts nearly every core clinical trial document. Managing this process requires a cross-functional, coordinated effort to maintain consistency and regulatory compliance. An unaligned amendment can compromise study integrity, as a change in one document necessitates synchronized updates across all related materials.
This coordinated effort is critical for aligning the Investigator's Brochure (IB), Informed Consent Forms (ICFs), Statistical Analysis Plan (SAP), and other key documents. Effective management ensures inspection readiness and upholds the operational and regulatory standards of the trial.
Why Coordinated Amendment Management Is Non-Negotiable
A protocol amendment should not be viewed as an isolated task. Amendments often arise from new safety data, regulatory feedback, or operational adjustments required for study conduct. Each change, regardless of its perceived scope, has downstream consequences for related clinical documentation.
An uncoordinated amendment process can introduce inconsistencies that compromise data integrity, create confusion for site staff, and potentially impact participant safety.
The Ripple Effect of a Single Change
Consider an amendment to tighten the inclusion criteria. This change extends beyond the protocol itself, directly affecting the Informed Consent Form, which must be updated to accurately reflect participant eligibility.
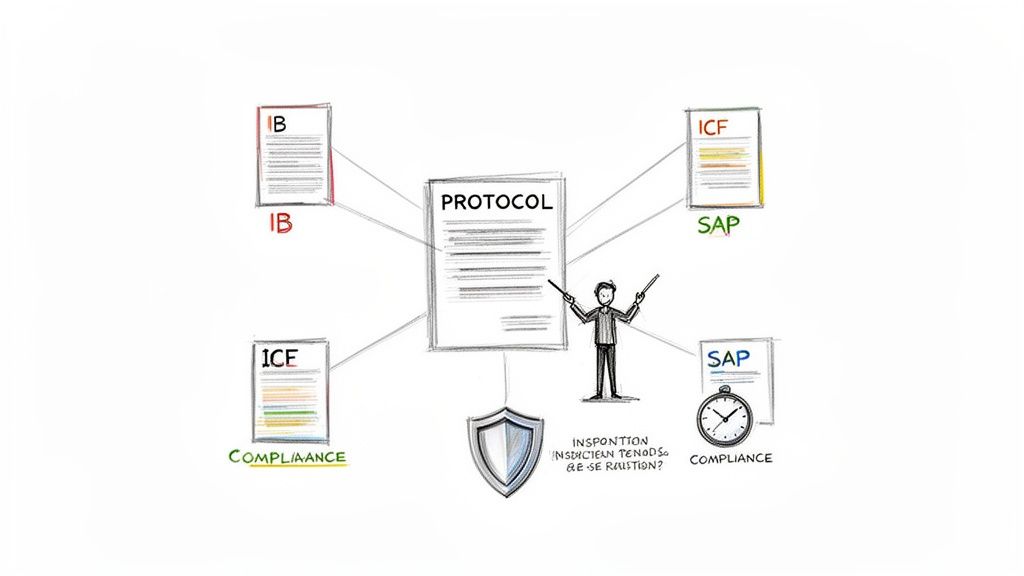
This cascade of updates must be synchronized through a meticulous change control process. This is not merely an administrative exercise but a core requirement for maintaining data integrity and protecting trial participants, consistent with principles outlined in guidelines such as ICH Good Clinical Practice (GCP).
The following table outlines common documents impacted by a protocol amendment.
Core Documents Affected by a Protocol Amendment
| Document | Reason for Impact | Common Updates Required |
|---|---|---|
| Informed Consent Form (ICF) | Directly impacts participant communication. | Revisions to procedures, risks, benefits, and eligibility criteria. |
| Investigator’s Brochure (IB) | Ensures investigators have the latest product info. | Integration of new safety, efficacy, or pharmacology data. |
| Statistical Analysis Plan (SAP) | Keeps the analysis aligned with the study design. | Changes to endpoints, analysis populations, or statistical methods. |
| Clinical Study Report (CSR) | Provides the final, accurate study narrative. | Documentation of all protocol versions and the rationale for changes. |
| Trial Master File (TMF/eTMF) | Creates a defensible audit trail. | Filing of approvals, submissions, training records, and communications. |
The protocol serves as the starting point. Each dependent document requires careful consideration and timely updates to maintain a cohesive and compliant record of the trial.
The Operational and Financial Burden of Amendments
Protocol amendments have become increasingly common. Industry data indicates that a significant majority of clinical trials now require at least one amendment.
The implementation process can also be lengthy. It takes, on average, several months to implement an amendment, during which sites may be required to manage multiple protocol versions. This operational complexity can lead to compliance risks, budget deviations, and increased workload for site staff. For those interested in the data, you can discover more insights about these amendment implementation inefficiencies.
A protocol amendment is not the end of a process but the beginning of a new one. It triggers a series of dependent workflows that, if not managed cohesively, can lead to critical compliance gaps discoverable during an inspection.
A systematic, proactive strategy for managing amendments across all clinical documentation is essential to protect the trial's integrity, maintain compliance, and ensure the well-being of study participants.
Building a Robust Change Control Framework
Effective management of protocol amendments begins with a well-defined governance framework. This structure ensures that every change is handled in a predictable, consistent, and auditable manner, preventing critical steps from being overlooked.
Without a formal change control process, teams may operate reactively. An amendment might be drafted without a thorough assessment of its budgetary or operational impact, leading to the last-minute discovery of numerous downstream document dependencies.
A strong framework transforms this potential chaos into a controlled workflow, aligning all functional areas and providing a clear line of sight from a proposed change through its final implementation.
Defining Roles and Responsibilities
Clarity regarding roles is fundamental. A well-defined governance structure specifies who has the authority to propose, review, approve, and execute protocol changes.
Key roles typically include:
- Change Initiator: Often a representative from Clinical Science or a Medical Monitor who identifies the need for an amendment and formally initiates the change control process.
- Impact Assessors: A cross-functional group from areas such as Clinical Operations, Regulatory Affairs, Data Management, Biostatistics, and Safety, who evaluate the proposed change from their respective domains.
- Reviewers: Subject matter experts who assess the technical and scientific details of the amended documents to ensure accuracy and consistency.
- Approvers: Senior leaders, such as the Head of Clinical Development, who provide final authorization for the amendment package to be implemented and submitted to regulatory authorities.
This structure ensures that decisions are not made in isolation and that individuals with the appropriate expertise contribute to the process.
Standardizing the Impact Assessment
Once roles are defined, the next step is to standardize the evaluation of a proposed change. This impact assessment is a critical component of the framework, compelling the team to consider the full consequences of an amendment before significant resources are invested.
An impact assessment isn't just an internal checklist; it's a crucial part of your Trial Master File (TMF). When an inspector comes knocking, this document shows them you have a deliberate process and provides a clear, defensible "why" behind every amendment.
The assessment should systematically cover key areas. For example, a seemingly simple modification to a secondary endpoint would require evaluation of its impact on:
| Area of Impact | Key Evaluation Questions |
|---|---|
| Scientific & Clinical | Does this alter the study's scientific validity? What are the implications for participant safety and the risk-benefit profile? |
| Operational | What is the operational burden for clinical sites? Will retraining be required? How will this affect study timelines or vendor contracts (e.g., IXRS, ePRO)? |
| Regulatory | Does this constitute a "substantial" amendment? Will new approvals be required from health authorities and Institutional Review Boards/Ethics Committees (IRBs/ECs)? |
| Documentation | Which specific documents require updates (e.g., ICF, IB, SAP, CSR shell)? What is the version control and distribution plan? |
Documenting this analysis creates a complete and defensible record of the decision-making process. A modern regulatory document management system can facilitate this by providing structured workflows and audit trails.
By making this process standard, every proposed change receives the same thorough vetting, ensuring consistency and inspection readiness.
Navigating the Cascade of Document Updates
A protocol amendment initiates a chain reaction, requiring updates across a network of interconnected clinical documents. Managing this cascade is a significant challenge in maintaining trial integrity and audit readiness.
Failure to manage this process effectively can lead to inconsistencies that confuse site staff, jeopardize data quality, and raise concerns during a regulatory inspection. The core principle is that every document must tell the same, consistent story. When the protocol changes, all dependent documents must be updated accordingly. This is fundamental to participant safety and the scientific validity of the trial.
Tracing the Impact from Protocol to Patient
Consider a scenario where an amendment is made to the inclusion/exclusion criteria to refine the target patient population. Once that amendment is approved, the current Informed Consent Form (ICF) is no longer valid. The ICF must be updated immediately to reflect the new eligibility criteria, ensuring that potential participants receive accurate information before providing consent.
Failure to synchronize the ICF with the protocol is a significant compliance issue that can undermine the ethical basis of the study and invalidate consent for participants enrolled with an outdated form.
This dependency extends to other key documents. For instance, an adjustment to safety monitoring procedures in the protocol has a direct impact elsewhere:
- Investigator’s Brochure (IB): If the amendment introduces new risk information or alters safety reporting procedures, the IB must be updated. Investigators require the most current information on the investigational product's safety profile.
- Statistical Analysis Plan (SAP): A change to a primary or secondary endpoint necessitates a corresponding update to the SAP. The plan for data analysis must align precisely with the objectives and endpoints defined in the protocol.
A robust change control process is essential for navigating these updates. The following flow chart illustrates a high-level workflow for initiating, assessing, and approving changes, which forms the backbone of managing the documentation cascade.
This type of process ensures that document updates are a planned outcome of a thorough assessment, with all impacts identified before work begins.
The Operational Challenge of Synchronization
A primary operational challenge is synchronizing the review, approval, and distribution of multiple updated documents. Managing parallel review cycles for the protocol amendment, the revised ICF, and the updated IB requires careful coordination between clinical operations, regulatory affairs, medical writing, and biostatistics.
A significant risk is the unintentional introduction of minor inconsistencies. For example, if a protocol amendment redefines a key study procedure, that exact language must be mirrored in the ICF and any related operational manuals for clinical sites. Even slight differences in terminology can create confusion and lead to documentation discrepancies.
At the end of the day, your goal is to present a completely cohesive and compliant story to regulatory bodies. Every updated document is a piece of that story, and they all have to fit together perfectly to show an auditor a clear, defensible sequence of events.
To achieve this, teams require a single source of truth for all information related to the amendment. This includes not only the final, approved documents but also the documented rationale for the change and the impact assessment that guided the update process. A clear understanding of the relationships between different regulatory documents in clinical trials is essential for successful amendment management.
Navigating this cascade requires proactive planning and meticulous execution. By mapping all dependencies, synchronizing workflows, and enforcing strict version control, a protocol amendment can strengthen a trial rather than introduce operational challenges.
Maintaining TMF Health and Inspection Readiness
The protocol amendment process concludes within the Trial Master File (TMF), the official record of the clinical trial. A TMF must provide a clear, complete, and contemporaneous account of all decisions made during the study. The final step in managing an amendment is ensuring the TMF accurately reflects the change and its full implementation.
This is an active process of filing every record related to the amendment to create a robust audit trail. A well-maintained TMF should enable an inspector to independently trace the entire sequence of events, from the initial discussion about the need for a change to the signed training logs from each clinical site.
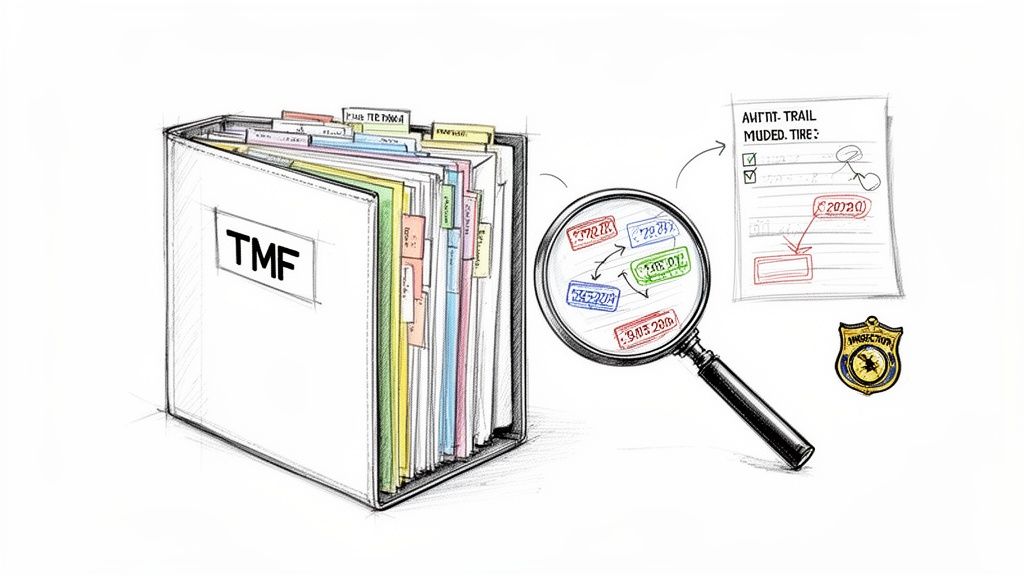
Building a Defensible Audit Trail in the TMF
Once an amendment is finalized, the focus shifts to documenting its lifecycle. The objective is to build an audit trail so clear that an inspector can follow it without requiring verbal explanation. This involves filing not just the final documents but also the contextual information surrounding the change.
A complete audit trail is composed of key artifacts:
- The Final, Approved Amendment: The signed, dated, and clearly versioned protocol amendment document.
- Regulatory & EC/IRB Submissions: Complete copies of all submission packages sent to health authorities and ethics committees.
- Approval Documentation: Official approval letters from all relevant regulatory bodies and ECs/IRBs for all sites.
- Updated Core Documents: The final, approved versions of the Informed Consent Form, Investigator's Brochure, SAP, and any other impacted documents.
- Communication Records: Evidence of notification to investigators and site staff, such as copies of emails, notification letters, or meeting minutes.
- Training Verification: Signed logs or certificates confirming that site personnel were trained on the new protocol version and procedures.
Adherence to a standardized framework like the TMF Reference Model helps ensure these artifacts are filed correctly, facilitating retrieval during an inspection.
The Challenge of Contemporaneous Filing
A common pitfall in TMF management is delayed filing. Good Clinical Practice (GCP) principles emphasize the importance of contemporaneous documentation. When amendment-related documents are filed weeks or months late, it creates gaps in the trial's narrative and may raise questions about study oversight during an inspection.
This poses a significant risk, particularly for pivotal trials that support regulatory submissions. The high frequency of amendments in later-phase trials necessitates efficient TMF processes to maintain a current and accurate record.
An inspector should be able to pick any patient visit in the eCRF, look at the date, and cross-reference the TMF to confirm exactly which protocol and ICF versions were active that day. A filing delay shatters that link and instantly erodes the TMF’s credibility.
Linking Documents to Tell the Whole Story
An effective TMF does more than store documents; it connects them to form a coherent narrative. An amendment is not a standalone event but part of the trial's ongoing story. Modern eTMF systems often allow for the creation of metadata links that illustrate the relationships between different documents.
For example, an EC approval letter for an amended ICF should be directly linked to the specific ICF version it approves. Site training records should be linked back to the protocol amendment that necessitated the training.
This network of connections transforms the TMF from a static repository into an intelligent record of compliance. This structured approach is fundamental to managing your Trial Master File and achieving true inspection readiness. By methodically documenting every step, teams can confidently demonstrate that each amendment was managed with the rigor and foresight that regulators expect.
Improving Cross-Functional Communication and Review
Ineffective communication is a common root cause of challenges in protocol amendment management. The process is not a linear task for a single department but an interconnected effort involving clinical operations, regulatory affairs, data management, medical writing, and clinical site personnel.
Without structured communication channels, review cycles can be prolonged, version control can be compromised, and inconsistent documents may result. This can lead to delays and errors.
Success depends on well-defined workflows, particularly for document review and feedback. Relying on email chains and shared folders is often insufficient, as it can lead to multiple "final" versions and a lack of a clear audit trail for decision-making. A system that captures, addresses, and formally resolves all feedback is essential.
Establishing Concurrent and Transparent Review Workflows
The objective is to facilitate a single, unified review of a group of related documents. When a protocol is amended, the ICF, Investigator's Brochure, and SAP are often impacted. These documents should ideally move through the review process together, in parallel.
This concurrent review allows, for instance, a biostatistician reviewing an updated SAP to simultaneously verify that new endpoint definitions align with the protocol. This approach helps identify cross-document inconsistencies that might be missed in siloed reviews.
A centralized platform that supports redlining and comment resolution can facilitate this process by enabling teams to:
- See Changes in Context: Reviewers can easily identify what has changed from the previous version, focusing their attention on the modifications.
- Settle Conflicting Feedback: A structured system can facilitate the resolution of differing opinions (e.g., between regulatory and clinical operations on ICF wording) and document the final decision.
- Keep a Single Source of Truth: All comments and resolutions are tied directly to the document text, eliminating the confusion of disparate email threads.
Proactive Planning to Minimize Preventable Amendments
The most effective way to manage an amendment is to prevent the need for it. A significant portion of amendments are not driven by new scientific data but by oversights that could have been identified during initial protocol design.
Industry research indicates that a notable percentage of all protocol changes are considered preventable. Proactively addressing potential issues during protocol development can reduce the number of avoidable amendments. Strategies in this area are explored in resources for learning more about proactive protocol writing.
A protocol amendment workflow is fundamentally a communication workflow. Its success is measured not just by the quality of the final documents, but by the clarity, efficiency, and auditability of the collaborative process that created them.
Ensuring Effective Dissemination to Clinical Sites
The final distribution of the approved amendment package to clinical sites is a critical step. A simple email with a PDF of the new protocol is often inadequate and can introduce compliance risks.
A clear, robust process is needed to disseminate this information to investigators and site coordinators. The package must be comprehensive and unambiguous.
Key elements for site dissemination include:
- A Clear Summary of Changes: A concise summary document highlighting the key changes that will affect day-to-day site operations.
- Version-Controlled Document Packet: All updated documents (e.g., Protocol v3.0, ICF v3.0, updated Pharmacy Manual v2.0) should be distributed together as a single package to ensure sites use the correct, synchronized set.
- Verifiable Training and Receipt: Formal, documented confirmation that the site has received the new documents and that staff have completed any required retraining. This documentation is a critical component of the TMF.
A systematic approach ensures that all personnel, from the sponsor's project manager to the site's research nurse, are working from the same set of approved documents.
Common Questions About Managing Protocol Amendments
When a protocol amendment is initiated, questions often arise from clinical, regulatory, and medical writing teams. This section addresses common queries with a focus on process and operational best practices.
What Is the First Step After Identifying the Need for an Amendment?
Before any text in the protocol is revised, the first step is to conduct a formal impact assessment. This foundational step helps validate the need for the change and prevents downstream operational challenges.
This involves convening a cross-functional team—typically including representatives from clinical science, regulatory affairs, data management, and safety—to systematically evaluate the potential effects of the proposed change. This assessment serves as the blueprint for the entire amendment process.
Key areas for evaluation include:
- Patient Safety and Data Integrity: How does the change affect the risk-benefit profile? Will it impact the scientific validity of the data being collected?
- Operational Execution: What is the operational burden on clinical sites? Will retraining be required? How will the change affect timelines and contracted vendors (e.g., IXRS, ePRO)?
- Budget and Resources: What are the estimated costs associated with implementing this change across all active sites?
- Downstream Documentation: Which specific documents will require updates? This typically includes the ICF, Investigator's Brochure (IB), Statistical Analysis Plan (SAP), and potentially the Clinical Study Report (CSR) shell.
Documenting this assessment provides a clear rationale for the change and serves as a critical artifact for the Trial Master File (TMF), demonstrating a controlled and thoughtful approach.
How Can We Ensure Consistency Across All Updated Documents?
Maintaining consistency across multiple updated documents requires a combination of disciplined processes and effective tools. Discrepancies in terminology, dates, or procedures are a common finding in audits and can cause confusion at clinical sites.
A best practice is to establish a single "source of truth" for core information, such as endpoint definitions or specific procedural instructions. When the protocol is amended, this source is updated first, and the change is then systematically cascaded to all dependent documents.
For teams relying on manual processes, a dedicated Quality Control (QC) step is essential. This final review should be conducted by an individual who was not involved in drafting the documents. They should use a detailed checklist to verify that all terminology, version numbers, and effective dates are identical across the protocol, ICF, and other related documents before distribution.
A common error is reviewing documents in isolation. The final QC process should always include a side-by-side comparison of the amended protocol against key dependent documents like the ICF and SAP to identify subtle but critical inconsistencies.
What Is the Most Common Global Management Mistake?
In multinational trials, a frequent mistake is underestimating the complexity of country-level implementation. A global amendment is not a single event but a series of coordinated local submissions, approvals, and rollouts, each with unique timelines and requirements.
Teams often do not allocate sufficient time for the variability in review timelines across different countries' regulatory bodies and ethics committees. This can lead to a staggered implementation where some sites operate on the new protocol version while others are delayed pending local approval.
To mitigate this, a robust global management plan is essential. This should include a country-specific tracker to monitor submission dates, approval status, and the planned implementation date for each site. Proactive communication with local teams or CRO partners is also critical to identify and address any country-specific documentation requirements—such as translated ICFs or additional local forms—in parallel. This foresight helps prevent bottlenecks and ensures a synchronized, compliant transition.