Structured document review and approval workflows in clinical trials are the operational framework for creating, verifying, and finalizing essential regulatory documents. These are not merely administrative procedures; they are core processes designed to ensure data integrity, maintain regulatory compliance, and establish a verifiable audit trail for every document, from initial draft to final archival.
The Foundation of Compliant Clinical Development
Robust document review and approval workflows are integral to the successful execution of any clinical trial. They are a fundamental requirement for ensuring data integrity, patient safety, and compliance with regulatory standards.
Every key document, from the clinical trial protocol to the final Clinical Study Report (CSR), undergoes a structured lifecycle of drafting, multidisciplinary review, and formal approval. A breakdown in this process can introduce significant risks, including potential inspection findings, submission delays, or compromised trial data that could jeopardize the entire study.
This structured approach is necessary to manage the complexity of clinical documentation. For example, a protocol amendment requires input from medical, statistical, clinical operations, and regulatory affairs personnel. A well-designed workflow ensures their feedback is incorporated in a controlled, sequential manner, preventing version control issues that arise from simultaneous, conflicting edits.
Managing Increased Complexity and Scrutiny
The need for disciplined workflows has intensified as clinical trials have become more complex and global in scope. An increase in trial initiation rates has led to a greater volume of regulatory documentation for sponsors and CROs, rendering manual or ad-hoc processes insufficient. Further details on this operational pressure can be found in more insights about this trend.
A disciplined workflow transforms document management from a reactive task into a proactive, strategic function. It provides verifiable evidence that established procedures were followed, which is essential for maintaining a state of inspection readiness.
Aligning Process with Regulatory Expectations
Guidelines from regulatory bodies such as the International Council for Harmonisation (ICH), the FDA, and the EMA emphasize the necessity of structured processes. While they do not mandate specific technologies, their core principles of quality, traceability, and accountability are intrinsically supported by well-defined review and approval systems.
An effective workflow captures every version, comment, and signature within a secure audit trail. This directly supports the regulatory mandate for data integrity and clear accountability. In modern clinical development, this systematic approach is a critical component of safeguarding the trial from inception to conclusion.
Architecting a Compliant Workflow Framework
A compliant workflow is more than a checklist; it is the blueprint for the entire documentation process. It defines roles, enforces a specific sequence of operations, and creates a robust audit trail. Process failures often originate from ambiguity in roles and responsibilities, which can lead to redundant reviews or missed oversight.
The first step is to clearly define roles within the document lifecycle. At a minimum, every workflow requires a designated Author, a set of Reviewers, and a final Approver, each with specific responsibilities.
This section breaks down what each role entails and its significance from a regulatory perspective.
Table: Key Roles and Responsibilities in a Clinical Document Workflow
This table outlines the distinct roles within a document review workflow, detailing their primary responsibilities and key regulatory considerations to ensure clear accountability.
| Role | Primary Responsibilities | Key Regulatory Considerations |
|---|---|---|
| Author | Creates the initial draft, integrates feedback from all reviewers, and is the primary driver of the document through the workflow. | Must be qualified and trained on the relevant SOPs and document templates. Their identity and actions must be captured in the audit trail. |
| Reviewer | Acts as a Subject Matter Expert (SME) to verify the accuracy, clarity, and compliance of content within their specific domain. | The delegation of authority log must show that reviewers are qualified for their area of expertise (e.g., medical, statistical, regulatory). |
| Approver | Provides the final, binding sign-off, confirming the document is complete, accurate, and ready for its intended purpose. | This is the formal acceptance of the document. The signature must comply with 21 CFR Part 11 or equivalent electronic signature regulations. |
Defining these roles is a fundamental tenet of Good Clinical Practice (GCP). Regulatory inspectors expect to see a clear, documented delineation of duties.
Risks of a Poorly Designed Workflow
Consider a biostatistician reviewing a Statistical Analysis Plan (SAP). This is not an informal suggestion; it is a formal validation of the study's statistical methodology. Their review is a critical quality control step, and the workflow must capture this action with appropriate formality.
Without this structure, significant risks can emerge.
This diagram illustrates the interconnectedness of workflow elements. A failure in version control compromises the audit trail's integrity and often leads to operational delays.
Designing Effective Review Gates
Once roles are defined, the next step is establishing review gates. A common error is distributing a document to all reviewers simultaneously ("parallel review"). This approach often generates a high volume of contradictory feedback, creating version control challenges for the author.
A sequential workflow offers a more controlled alternative.
A key advantage of a sequential workflow is that it establishes foundational agreement before finer details are examined. For example, the clinical and medical teams can finalize the core scientific content of a protocol before it is sent to regulatory affairs for a final compliance review.
For a complex protocol amendment, a structured, sequential workflow could be:
- Round 1: Medical & Clinical Operations. The core team validates the scientific rationale and operational feasibility.
- Round 2: Statistics. Once core changes are stable, the biostatistician confirms the amendment does not compromise the trial's statistical integrity.
- Round 3: QA & Regulatory. With scientific and operational elements established, the QA and regulatory teams conduct a final review for alignment with internal SOPs and global regulations.
This phased approach prevents downstream reviewers from spending time on sections that are still undergoing significant changes, improving overall efficiency. These individual workflows are a component of the broader discipline of clinical trial document lifecycle management.
The Importance of Codified SOPs
Finally, all workflows must be codified in Standard Operating Procedures (SOPs). A workflow that exists only through informal communication is not defensible during an audit.
SOPs must explicitly document the roles, review sequences, and systems used for each major document type, from protocols and ICFs to the final CSR. This documentation transforms an ad-hoc process into a repeatable, scalable, and compliant system, serving as both a training tool and the standard against which operations are measured during an inspection.
Leveraging Technology for Efficiency and Oversight
Manual, fragmented workflows are a significant source of operational friction in clinical trials. Reliance on email chains, shared drives, and spreadsheets for document review introduces risks to data integrity and version control. This approach makes it difficult to maintain the clear, contemporaneous audit trail required by regulators.
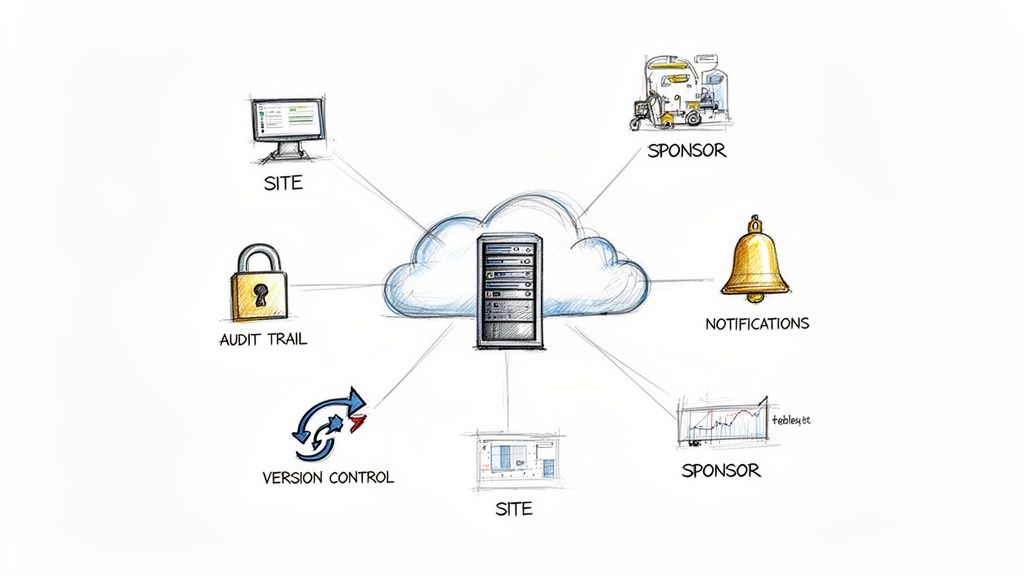
Modern technology addresses these challenges by consolidating document review and approval workflows in clinical trials into a single, controlled platform. The goal is not technology adoption for its own sake, but rather the use of specialized tools to enforce procedural discipline as expected by regulatory bodies. A centralized system can transform a chaotic process into one that is structured, transparent, and defensible.
Overcoming Common Operational Hurdles
A protocol amendment distributed for review via email can quickly lead to multiple, conflicting versions. The author must then spend considerable time reconciling feedback rather than focusing on scientific content, directly impacting study timelines.
The disconnect between sites and sponsors can exacerbate these issues. Industry analyses indicate that site-level data management challenges can cause operational drag throughout the document review cycle. An analysis referenced in a 2025 clinical trial trends analysis on CenterWatch noted that a significant percentage of sites report delays due to communication issues and continue to use email for document exchange, often while managing multiple disparate platforms.
A purpose-built platform can address these problems by:
- Establishing a single source of truth: All stakeholders work from the same document version.
- Automating reviewer notifications: The system prompts the next individual in the sequence, helping to prevent bottlenecks.
- Providing real-time visibility: Study managers can monitor a document's status without manual follow-up.
The Role of an Immutable Audit Trail
From a regulatory perspective, the most critical function of a technology platform is the creation of an immutable, time-stamped audit trail. Every action—document creation, version updates, comments, and electronic signatures—is automatically logged. This provides a complete, verifiable history of the document's lifecycle.
A regulatory inspector needs to see not only the final, approved document but also the complete history of its development—who reviewed it, what changes were made, and who provided final sign-off. A robust technological system provides this history with clarity and accuracy.
This automated record-keeping directly supports regulations such as FDA 21 CFR Part 11, which governs electronic records and signatures. It minimizes human error in maintaining logs and ensures a document’s history is always complete. For more information on this topic, refer to this guide on building a regulatory document management system.
Shifting Focus from Administration to Quality
Ultimately, technology-enabled workflows allow teams to focus on the scientific and regulatory quality of the documentation rather than administrative tasks.
When workflows are automated and transparent, medical writers, statisticians, and regulatory affairs experts can apply their expertise to the content itself, not to managing file versions or tracking signatures. This shift allows for more thorough reviews and higher-quality final documents. By reducing the friction of manual processes, teams can work more effectively, maintain compliance, and finalize critical trial documentation more efficiently.
Aligning Workflows with Key Regulatory Mandates
A well-designed workflow is an operational demonstration of regulatory compliance. Authorities like the FDA and EMA, along with guidelines such as ICH GCP, define the expected outcomes of a compliant process: data integrity, traceability, and accountability. A thoughtfully constructed document review workflow is designed to produce these outcomes.
Each step in the review process should correspond to a regulatory requirement. When a reviewer adds a comment or a manager applies an electronic signature, the system is not just completing a task; it is generating the evidence an auditor will require to verify that processes are deliberate and controlled.
Translating 21 CFR Part 11 into Workflow Design
The FDA's 21 CFR Part 11 establishes the criteria for trustworthy electronic records and signatures. A structured workflow is a practical method for implementing these requirements.
Specific workflow features can be mapped directly to the regulation's core tenets:
- Audit Trails: Part 11 requires secure, computer-generated, time-stamped audit trails that log all operator actions. A compliant workflow system automates this, capturing who authored, reviewed, commented on, and approved a document.
- Electronic Signatures: The regulation specifies that electronic signatures must be unique to an individual and not reusable. A workflow should enforce this by linking a signature to a specific version of a document, permanently associating that approval with that exact content.
- Access Controls: Workflows must operate within a system that has robust access controls, ensuring that only authorized individuals can perform specific actions, such as applying a final signature.
A workflow that enforces a specific sequence of review and approval is a direct demonstration of adherence to 21 CFR Part 11 principles, showing a controlled process where every action is attributable and logged.
Embedding ICH E6(R3) Principles of Quality and Risk
The evolution of ICH Good Clinical Practice (GCP), particularly with ICH E6(R3), promotes a proactive, risk-based approach to trial management. This includes applying quality-by-design principles to operational processes, such as document review workflows.
Instead of a single, rigid review process, workflows can be designed to match the risk and complexity of the document. For example, a minor correction in a site-facing manual may only require a two-person review, whereas a protocol amendment with potential patient safety implications should trigger a more rigorous, multi-stage workflow involving medical, statistical, and regulatory experts. A robust change control process is critical, and you can learn more about managing change control in clinical trial documentation.
A Practical Example: The Clinical Study Report (CSR)
The Clinical Study Report (CSR) is a critical document that forms the basis of a regulatory submission. A compliant workflow for a CSR might look like this:
- Drafting and Internal Review: The author drafts the CSR, and the workflow routes it to the core clinical and biostatistics teams for initial review. All comments and edits are captured in the audit trail.
- Cross-Functional Validation: Once the data and key narratives are stable, the workflow directs the document to other functions, such as pharmacovigilance and regulatory affairs. This gated approach prevents stakeholders from reviewing content that is still undergoing significant change.
- Quality Assurance (QA) Review: Before final approval, the workflow sends the CSR to the QA team. Their role is to verify that the report's structure, content, and formatting align with ICH E3 guidelines and internal SOPs.
- Final Approval and Signature: Finally, the workflow routes the finalized CSR to the designated approver(s). Their 21 CFR Part 11-compliant electronic signature is applied, which locks the document, generates the final version, and archives it as the official record for submission.
From start to finish, the process is managed by the workflow, creating a complete, auditable history that demonstrates a controlled, compliant, and quality-driven approach.
Measuring Performance and Driving Continuous Improvement
A workflow requires ongoing monitoring and refinement to remain effective and compliant. Continuous improvement allows for adaptation to new challenges and maintains a state of inspection readiness.
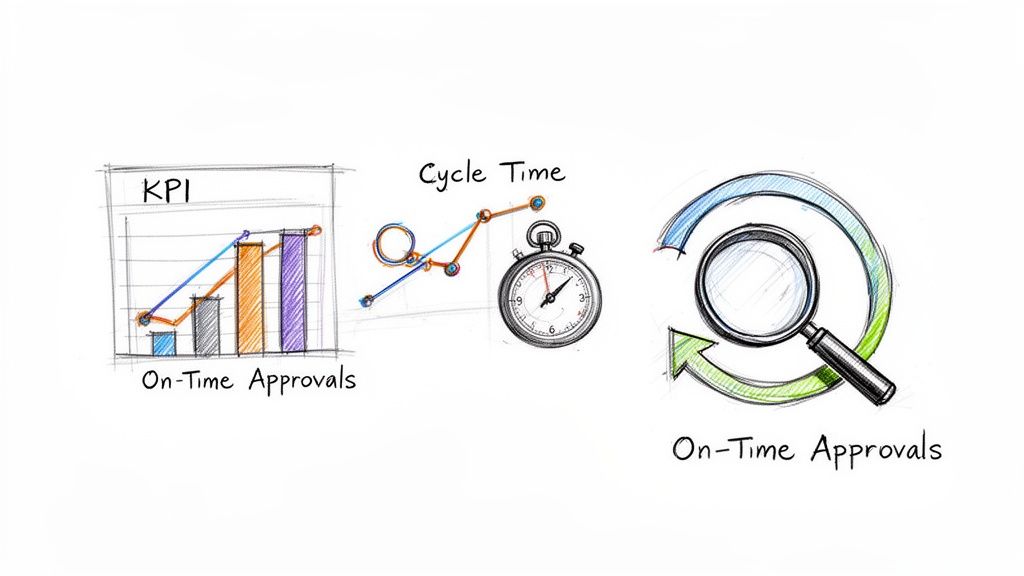
This process is founded on performance data. By tracking relevant Key Performance Indicators (KPIs), organizations can move from subjective assessments to evidence-based decisions that address real bottlenecks.
Defining Meaningful Workflow KPIs
KPIs should measure both efficiency and quality. A balanced set of metrics provides a comprehensive view of workflow performance.
Core metrics to monitor include:
- Average Review Cycle Time: The total time from initiation to final approval, analyzed by document type (e.g., protocol vs. ICF) to identify delays.
- Number of Review Rounds: The frequency with which a document is returned for revisions. A high number for a specific document type may indicate issues with initial guidance or authoring templates.
- Rate of On-Time Approvals: The percentage of documents approved by their scheduled deadline, measuring adherence to project milestones.
- Time Spent at Each Review Gate: This metric helps pinpoint where documents are delayed by tracking the duration they spend with each reviewer or department.
Interpreting Data to Identify Bottlenecks
Data analysis reveals patterns that point to process deficiencies. A long review cycle is a symptom of an underlying problem.
For example, if Statistical Analysis Plans (SAPs) are consistently delayed during medical review, the root cause may not be reviewer speed but a lack of initial clarity. A potential solution could be a kickoff meeting between the author and key reviewers to align on objectives before the formal review begins.
A continuous improvement loop is about systematically removing process friction. Using KPIs ensures that changes are data-driven solutions to well-defined problems.
Creating a Continuous Improvement Loop
This data-driven approach fosters a culture of continuous improvement. Insights from KPIs should inform updates to SOPs, workflow configurations, and team training. This creates a feedback loop: operational data drives process enhancements, which in turn improve workflow efficiency and resilience.
The impact of such optimization can be substantial. For example, the UK's MHRA reduced the average approval time for clinical trials by a reported 55% through a combination of process redesign and new technology, while maintaining safety standards. These results, about which you can discover more about these impactful findings on Digital Health, demonstrate how strategic, data-guided optimization can yield significant operational benefits.
Frequently Asked Questions About Document Workflows
The following are common questions from clinical operations teams regarding the management of clinical trial documents, with answers grounded in operational experience and regulatory principles.
What is the most common bottleneck in document review?
The most frequent bottleneck is inefficient feedback management. This occurs when an author distributes a document to multiple reviewers via email and receives separate, often conflicting, marked-up files in return. The author must then spend significant time reconciling these comments into a single, coherent document, leading to version control issues and missed deadlines.
The solution is to use a centralized platform that establishes a single source of truth. A well-designed system enforces a controlled workflow, whether sequential or structured parallel review. This prevents stakeholders from editing separate copies simultaneously. All comments are made in one location, visible to all parties, which simplifies and accelerates the reconciliation process.
How can approval workflows be made audit-ready?
Audit readiness depends on a complete and immutable audit trail, a core requirement of standards like FDA 21 CFR Part 11. The system must capture every interaction with a document—authorship, review, comments, and approval—with a precise, unalterable timestamp.
Electronic signatures are a critical component. They must be cryptographically linked to the specific document version that was signed, creating an unbroken chain of evidence. An inspector needs to see that SOPs were followed and that every action is clearly attributable to a specific individual at a specific time. A validated electronic system is the only reliable method for producing this evidence on demand.
An auditor's objective is to reconstruct a document's history. A system with a complete, tamper-proof audit trail provides this history, demonstrating a state of continuous control.
What is the difference between a "review" and an "approval"?
This is a critical distinction for establishing clear accountability within document review and approval workflows in clinical trials.
- A review is the act of providing expert feedback. A statistician reviews an analysis plan for technical accuracy, or a medical monitor reviews a safety reporting section for clinical soundness. Their input is an advisory quality check.
- An approval is the final, binding sign-off. It is the formal acceptance of responsibility for the document by an authorized individual, such as a Principal Investigator or department head. This signifies that the document is correct, complete, and ready for its intended purpose.
The workflow must make this distinction clear. An approval typically requires a compliant electronic signature for formal validation. A document is not considered final or effective until all designated approvers have provided their signature.
Should different workflows be used for different document types?
Yes, this is a recommended practice. Applying the same rigid, multi-step workflow to all documents, regardless of complexity, is inefficient.
A risk-based approach allows for workflows tailored to the document's importance.
- High-Impact Documents: Protocols, Investigator's Brochures (IBs), and Clinical Study Reports (CSRs) require a formal, sequential review process involving medical, statistical, regulatory, and QA functions.
- Medium-Impact Documents: For documents like a Statistical Analysis Plan (SAP) or a pharmacy manual, a more focused workflow involving only key subject matter experts may be appropriate.
- Low-Impact Documents: Internal training guides or simple administrative logs can often be managed with a streamlined two-step review and approval process.
By tailoring the workflow, the level of scrutiny matches the document's potential impact on the trial and patient safety. This aligns with the risk-based management principles emphasized in regulatory guidance such as ICH E6(R3).