Change control is the formal, structured process for proposing, assessing, approving, implementing, and verifying modifications to critical documents in a clinical trial. This is a systematic approach to ensure every modification—from a minor clarification to a major protocol amendment—is managed to maintain patient safety, data integrity, and regulatory compliance.
Why Change Control Is a Pillar of Trial Integrity
The principle "if it isn't documented, it didn't happen" highlights the importance of meticulous records in clinical research. An equally important principle is that if a document is changed without a formal process, its integrity is compromised. This is why the discipline of change control is a fundamental component of any quality management system.
An effective way to conceptualize change control is as an air traffic control system for clinical trial documents. Air traffic controllers track every deviation from a flight plan to prevent adverse events. Similarly, a change control process meticulously tracks every modification to a document, ensuring the scientific and ethical basis of the trial remains stable. Without it, uncontrolled changes can introduce significant risks.
The Core Purpose of Change Control
At its core, change control in clinical trial documentation is about maintaining a state of control over the documents that define and direct a study. It creates a defensible record explaining why a document evolved over time—a record that is essential during regulatory inspections. Uncontrolled updates to the protocol or Investigator's Brochure could create a domino effect of negative consequences, threatening data reliability, regulatory submissions, and participant safety.
This is not an administrative exercise; it is a core requirement outlined in guidelines like ICH E6(R2), which specifies the sponsor's responsibility for implementing and maintaining quality assurance and quality control systems. A robust change control process is a tangible demonstration of that oversight.
Documents Under Formal Change Control
While a trial generates numerous documents, a specific set of high-impact documents must be managed under formal change control. These typically include:
- Clinical Trial Protocol: The document detailing the study's objectives, design, methodology, and statistical approach.
- Investigator's Brochure (IB): The compilation of clinical and nonclinical data on the investigational product.
- Informed Consent Form (ICF): The document used to inform potential participants about the trial and obtain their consent.
- Statistical Analysis Plan (SAP): The pre-specified plan for how the trial data will be analyzed.
- Clinical Study Report (CSR): The comprehensive report presenting the trial’s methods and results.
The primary objective of change control is to ensure that modifications are intentional, justified, reviewed by appropriate stakeholders, and documented in a way that provides a complete, traceable history for inspectors and auditors.
Evolving regulatory expectations have shifted focus from simply documenting compliance to demonstrating 'provable control.' This means regulators expect to see traceable evidence that risks associated with document changes were actively identified, monitored, and addressed, impacting everything from site monitoring to data cleaning and audits. You can find more insights about evolving regulatory expectations and their impact on trials.
Every sound change control process, whether manual or automated, follows a logical progression. The following table breaks down the essential stages.
Core Components of a Change Control Process
| Process Step | Objective and Key Activities |
|---|---|
| 1. Change Request | To formally initiate and justify the need for a change. This involves completing a change request form, detailing the proposed modification, its rationale, and its potential impact. |
| 2. Impact Assessment | To evaluate the proposed change from clinical, regulatory, operational, and statistical perspectives. Subject matter experts assess how the change might affect timelines, budget, patient safety, and other documents. |
| 3. Review and Approval | To secure formal sign-off from all relevant stakeholders. A designated review board or group of approvers examines the request and the impact assessment before granting approval. |
| 4. Implementation | To execute the approved change accurately. This involves updating the document, assigning a new version number, and ensuring the changes are correctly reflected. |
| 5. Verification and Closure | To confirm the change was implemented correctly and effectively. This step includes quality checks and updating the change log before formally closing the request. |
| 6. Communication | To notify all affected parties that a change has been made. This ensures all stakeholders, from the study team to the clinical sites, are working from the most current, approved version of the document. |
Each of these steps works together to create a closed-loop system, ensuring that every change is managed with the rigor that clinical research requires.
Understanding the Regulatory Landscape for Change Control
Regulatory bodies such as the FDA and EMA provide the foundational principles for change control rather than a detailed procedural manual. Understanding the intent behind these regulations allows for the development of practical workflows that are both operationally effective and compliant with audit standards.
This perspective moves an organization from a "check-the-box" mentality towards a risk-based approach to quality management.
The two main pillars supporting a compliant change control process are the International Council for Harmonisation (ICH) Good Clinical Practice (GCP) guidelines and the FDA's regulations for electronic systems.
What ICH E6(R2) Really Expects
At its core, ICH E6(R2) emphasizes sponsor oversight and the implementation of a robust quality management system (QMS). While the term "change control" is not explicitly repeated throughout, its principles are integral to the guideline's focus on maintaining trial integrity and data quality.
ICH E6(R2) establishes that the sponsor is ultimately responsible for ensuring that all processes are sound and well-documented.
A well-defined process for change control in clinical trial documentation is how a sponsor demonstrates it is meeting that responsibility. It is the tangible evidence that a system is in place to manage changes to critical documents, preventing unapproved or unvetted updates that could compromise the study's scientific credibility or participant safety.
From an auditor's perspective, an uncontrolled change is an undocumented risk. The change control process is the mechanism that demonstrates the ability to identify, evaluate, and manage the risks associated with modifying essential trial documents.
The Critical Role of FDA 21 CFR Part 11
When clinical trial documents are managed electronically, FDA 21 CFR Part 11 becomes applicable. This regulation sets the requirements for ensuring electronic records and signatures are as trustworthy and reliable as their paper equivalents. You can explore these requirements in more detail in this comprehensive guide on FDA 21 CFR Part 11 compliance.
In the context of change control, Part 11 requires specific system capabilities:
- Secure Audit Trails: The system must automatically create a secure, computer-generated, time-stamped audit trail. This log must record all actions that create, modify, or delete an electronic record, capturing the "who, what, when, and why" for every change. It must be uneditable.
- Version Control: The platform must be able to manage different document versions. This ensures that stakeholders use the current, approved version while maintaining a complete history of all previous versions for traceability.
- Controlled Access: System access must be restricted. Specific user roles and permissions must be assigned to prevent unauthorized modifications to documents.
These global standards set a clear, unified expectation for how documentation changes are handled, which is particularly important for multinational trials. Robust change control is essential for maintaining data integrity.
For context, a recent analysis showed that in only 3.2% of global randomized clinical trials published between 2013 and 2021 in top journals, data was sent to lower or middle-income countries for analysis. This data flow from the Global South to the Global North underscores the importance of having robust change control processes that can track and verify modifications as data moves across international borders.
Building a Compliant and Practical Change Control Workflow
A sound change control process is the essential framework that ensures every change to a critical document is handled with consistency and foresight. This workflow must be effective whether implemented on paper, in a hybrid system, or on a fully digital platform, providing all stakeholders with a clear process to follow.
The objective is to break down a complex regulatory requirement into a series of logical, manageable steps. By moving from one phase to the next, every proposed change is properly vetted before it is implemented, protecting the integrity of the trial.
This is how high-level regulatory principles from ICH E6(R2) and FDA 21 CFR 11 are translated into the day-to-day operational workflows that maintain documentation compliance.
As illustrated, operational processes serve as the bridge connecting regulatory principles to compliant execution. This ensures daily tasks align with global standards.
The Five Phases of an Effective Workflow
An effective workflow for change control in clinical trial documentation is built on five core phases. This closed-loop system creates a complete and auditable history for every change made.
-
Change Request Initiation: A stakeholder identifies a need for a change and completes a standard change request form. This initial step captures the "what" and the "why," providing a clear justification for the change.
-
Impact Assessment: A cross-functional team evaluates the potential consequences of the proposed change. This is a critical analytical step that considers the ripple effects across the entire study.
-
Formal Review and Approval: The request package is submitted to a pre-defined group of approvers. This group, often comprising representatives from quality, regulatory, and clinical operations, has the authority to approve or reject the change based on the evidence presented.
-
Controlled Implementation: Once approved, the change is executed. This involves updating the document, assigning a new version number according to standard operating procedures (SOPs), and verifying that all modifications are implemented precisely as approved.
-
Verification and Closure: The final step confirms that the change was implemented correctly and communicated to all relevant parties. The updated document undergoes a final quality check, any necessary training is delivered, and the official change control record is formally closed.
The goal of a structured workflow is not to prevent change, but to manage it. It ensures every modification is intentional, justified, and implemented in a way that minimizes risk to patient safety and data integrity.
Detailing the Impact Assessment Phase
The impact assessment phase is critically important, as a superficial assessment is a common vulnerability in a change control system. A thorough evaluation analyzes the potential effects across several key areas. To understand how this fits into the broader context, review this guide on clinical trial document lifecycle management.
A robust assessment should address questions such as:
- Patient Safety: Could this change introduce a new risk to trial participants?
- Data Integrity: Will this modification affect how data is collected, analyzed, or reported?
- Regulatory Compliance: Does the change maintain alignment with GCP and other applicable regulations?
- Dependent Documents: What other documents (e.g., ICFs, lab manuals, training materials) will also require updates?
- Budget and Timelines: What are the time and resource implications? Could it delay major study milestones?
- Operational Execution: How will this affect clinical sites, monitors, or vendors?
By methodically progressing through these five phases—and conducting a thorough impact assessment—an organization can build a change control process that is both audit-ready and operationally efficient.
Ensuring Traceability with Versioning and Audit Trails
If the change control process is the engine of compliance, then versioning and audit trails are its structural frame. These two components work together to create a complete, unbroken record showing what changed in a document, along with the how, when, who, and why behind it. For a regulatory inspector, this level of traceability is the necessary proof that processes are under control.
Systematic versioning provides a clear, sequential history of a document's lifecycle. Proper implementation eliminates the confusion of multiple drafts and reduces the risk of teams working from outdated information—a scenario that can impact everything from patient consent to final data analysis.
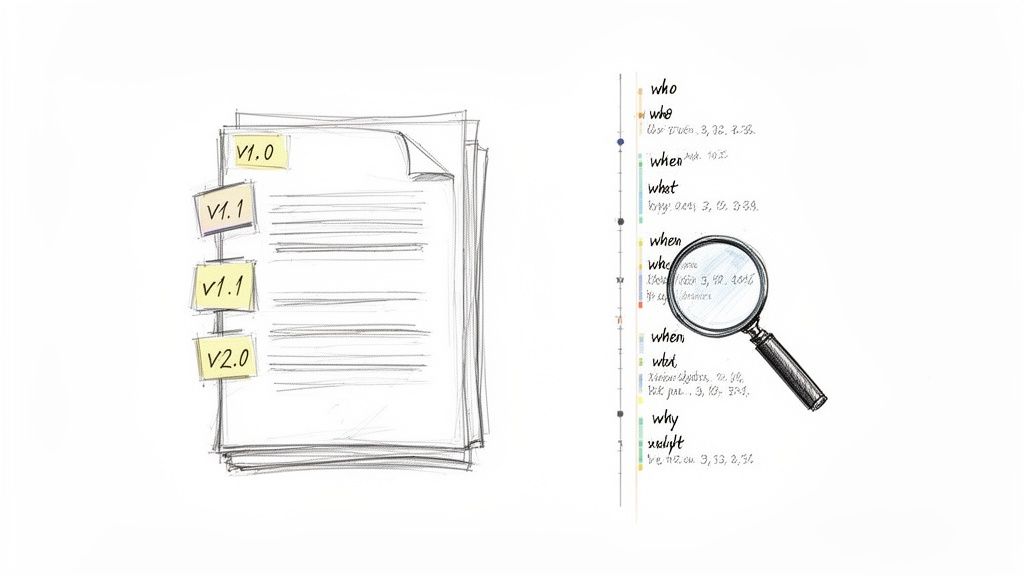
Differentiating Minor and Major Versions
A sound versioning system, clearly defined in an SOP, provides clarity. It distinguishes between minor corrections and significant revisions, a distinction that is important for both internal teams and external auditors.
-
Minor Versions (e.g., v1.1, v1.2): These represent minor edits that do not alter the core meaning or scientific intent of the document, such as correcting typographical errors, clarifying wording, or adjusting formatting. These changes typically follow a simplified review process.
-
Major Versions (e.g., v2.0, v3.0): These signify a substantive change that could impact study conduct, patient safety, or data integrity. Amending a protocol to add a new patient cohort or change a primary endpoint constitutes a major version update and requires the full, formal change control workflow.
This approach is effective because the version number itself communicates the magnitude of the change.
The Audit Trail: An Indisputable Record of Every Action
While versioning shows the high-level evolution of a document, the audit trail provides the forensic details. It is the unchangeable, time-stamped log of every action related to that file. In a system compliant with regulations like FDA 21 CFR Part 11, this trail is generated automatically and cannot be altered. It serves as the definitive source of truth.
An audit trail transforms change control from a theoretical process into a demonstrable reality. It is the objective evidence that proves every modification was deliberate, reviewed, and justified, satisfying the core principles of data integrity and sponsor oversight.
This meticulous record-keeping is increasingly important as clinical trials become more global. There is a significant push for international standards through guidelines like ICH E6(R3), which emphasizes consistency in change control in clinical trial documentation. With data from ClinicalTrials.gov showing that 50% of all studies (172,209) are now conducted outside the U.S., the need for robust, unified change processes that function across borders has never been greater. You can discover more insights about global clinical trial data standardization and its growing impact on the industry.
To illustrate how this works in practice, let's examine how change control applies to some of the most critical documents in a trial.
Change Control Scenarios for Core Clinical Documents
| Document Type | Common Change Trigger | Key Change Control Actions |
|---|---|---|
| Investigator's Brochure (IB) | New pre-clinical safety data emerges. | Initiate change request, convene safety committee for impact assessment, update IB to a new major version, notify all investigators and ethics committees, and document training. |
| Informed Consent Form (ICF) | Protocol amendment adds a new study procedure. | Revise ICF to include new procedure risks/benefits, obtain IRB/EC approval for the new version, manage re-consent of existing participants, and ensure all sites use only the new approved version. |
| Clinical Study Protocol | An interim analysis suggests a dosing change is needed. | Draft protocol amendment, circulate for multi-departmental review (e.g., statisticians, clinicians, regulatory), submit to regulators and IRBs, finalize as a new major version, and retrain all site staff. |
| Statistical Analysis Plan (SAP) | Blinding is broken prematurely for a safety review. | Document the unblinding event and justification, potentially revise SAP to account for the event, secure approval from study leadership, and lock the updated SAP before final analysis. |
These examples show that change control is not a single action but a cascade of documented, deliberate steps tailored to the specific document and the reason for the change.
Example: A Compliant Audit Trail for a Protocol Amendment
Consider a protocol amendment approved to tighten patient eligibility criteria. As a major change, the document version would advance from v2.0 to v3.0. A compliant, automated audit trail would capture every step of this process:
- Change Request:
[Timestamp] User [Clinical Lead] initiated Change Request #123 for Protocol XYZ. - Document Checkout:
[Timestamp] User [Medical Writer] checked out Protocol XYZ v2.0 for editing. - Modification:
[Timestamp] User [Medical Writer] edited Section 4.1 'Inclusion Criteria' and saved as draft v2.1. - Submission for Approval:
[Timestamp] User [Medical Writer] submitted draft v2.1 for review and approval. - Stakeholder Review:
[Timestamp] User [Regulatory Affairs] approved draft v2.1. Reason: 'Changes align with regulatory feedback.' - Final Approval:
[Timestamp] User [Chief Medical Officer] provided final e-signature approval. - Version Finalization:
[Timestamp] System automatically finalized and published Protocol XYZ as v3.0.
This granular log provides a clear, step-by-step record, demonstrating that the change was managed through a formal, compliant, and fully documented process.
Common Change Control Pitfalls and How to Avoid Them
Even with a well-defined Standard Operating Procedure (SOP), the practical application of change control can present challenges. Common issues can create compliance gaps that may not be identified until a regulatory inspection. Proactively addressing these weaknesses is essential for maintaining an audit-ready state.
Often, problems arise not from a flawed procedure but from small shortcuts and inconsistent practices that emerge under operational pressure.
Informal Approvals and "Hallway" Decisions
A significant risk is allowing critical decisions to be made via email or informal meetings. A verbal approval or a brief note in a long email chain may seem efficient, but it lacks the traceability required for an audit.
From a regulatory standpoint, an undocumented change is an uncontrolled one. It directly contravenes the core principles of Good Documentation Practice (GDP), which require every action to be attributable, legible, contemporaneous, original, and accurate (ALCOA).
The solution is to make the formal process the most straightforward path. A user-friendly electronic system where stakeholders can log, track, and approve change requests within a validated environment reduces the incentive for informal workarounds. Compliance becomes more natural when the correct process is also the simplest.
The Underestimated Impact Assessment
Another common pitfall is the superficial impact assessment. This occurs when a team modifies one document without considering its connections to others. For example, a protocol amendment that alters the patient visit schedule necessitates updates to the Informed Consent Form, site training materials, and potentially the Statistical Analysis Plan.
Failure to identify these dependencies creates a cascade of mismatched information across the Trial Master File (TMF). This not only introduces a significant compliance risk but also causes operational confusion for clinical site staff. A rushed assessment is not just a procedural shortcut; it disables a critical risk management feature of the quality system.
The true test of a change control system is not how it handles a single document, but how it manages the web of interconnected information. A thorough impact assessment is a risk management tool that prevents a minor update from causing a systemic failure.
To avoid this, integrate a mandatory impact assessment checklist into the change request form. This prompts the team to systematically consider the effects on:
- Dependent Documents: List which other documents (e.g., ICFs, lab manuals) may require corresponding updates.
- Site Operations: How will the change affect clinical sites, vendors, or the patient experience?
- Budgets and Timelines: What are the resource implications of implementing the change?
- Regulatory Submissions: Does this change need to be reported to the FDA, EMA, or an ethics committee?
Inconsistent Training and Enforcement
Finally, even a well-designed SOP is ineffective if the team does not understand its application or importance. A common audit finding is the inconsistent application of change control in clinical trial documentation across different studies. This typically arises when new team members are not properly onboarded or when long-serving staff develop ad-hoc workarounds.
The solution is consistent, role-specific training. This should be an ongoing part of professional development, reinforced with real-world examples illustrating the consequences of procedural deviations.
To ensure consistency, a central Quality Assurance group should perform periodic internal reviews. This helps confirm that the process is being followed uniformly, maintaining a single standard of quality across the organization.
How Technology Reinforces Compliant Change Control
Manual, paper-based change control processes are susceptible to human error. They place a significant burden on individuals to follow every step, route documents correctly, and log every action. This is often not a sustainable model for modern clinical trials.
Technology can mitigate these risks by embedding the rules of compliant change control in clinical trial documentation directly into the digital workflow. This makes adherence to the process the default rather than the exception.
A purpose-built platform does more than store files; it actively enforces SOPs. By automating critical steps, it reduces administrative workload while strengthening oversight. This allows the team to focus on the scientific and ethical rationale for a change, while the system manages procedural details in a compliant, verifiable manner.
Automating Core Compliance Functions
Technology can hardwire compliance into daily tasks. A system designed with standards like ICH GCP and FDA 21 CFR Part 11 in mind creates a structured environment where the correct process is also the most efficient one.
This is what that looks like in practice:
- Role-Based Permissions: The system ensures that only authorized individuals can initiate, review, approve, or implement changes. These access controls are a primary defense against unauthorized edits and a cornerstone of data integrity.
- Automated Versioning: Upon approval, the platform automatically finalizes the document as the new official version (e.g., v2.0), archives the previous version, and establishes the new one as the single source of truth.
- Integrated Electronic Signatures: Compliant e-signatures are built into the approval workflow. They are securely linked to the document and timestamped, creating a legally binding record.
Establishing an Immutable Single Source of Truth
Ensuring all stakeholders are working from the same set of documents is a major challenge in trial management. A stray email attachment can lead to significant discrepancies. Technology addresses this by creating a central, validated repository where sponsors, CROs, and sites access the same current, approved documents.
A purpose-built platform acts as the definitive source of truth. By eliminating the possibility of multiple, conflicting versions circulating via email, it eradicates a major source of compliance risk and operational confusion.
This controlled environment is supported by an immutable audit trail. Every action—from viewing a document to adding a comment or applying a signature—is automatically logged with user, date, and time stamps. This computer-generated log cannot be altered, providing inspectors with objective, verifiable proof that the change control process was followed. You can explore how these features are integrated within a specialized regulatory document management system.
By building these controls into its foundation, technology transforms change control from a cumbersome manual process into an efficient, automated quality function. This not only prepares an organization for inspection but also provides a robust, defensible history of every decision made for every document throughout the trial lifecycle.
Common Questions About Change Control
The practical application of change control in a clinical trial can raise several questions for study teams. Here are answers to some of the most common inquiries.
What's the Difference Between Version Control and Change Control?
These two concepts are closely related but distinct. Version control is the what, and change control is the why.
Version control is the technical system for labeling documents (e.g., v1.0, v1.1, v2.0). It is the mechanism for tracking the evolution of a document from one iteration to the next.
Change control is the formal quality process that governs versioning. It encompasses the entire lifecycle of a modification: the formal request, the impact assessment, the multi-stakeholder review, the official approval, and the documented justification for why the change was necessary. An auditor requires not just the new version number, but the complete, documented history that the change control process provides.
Does Every Typographical Error Require the Full Process?
Not necessarily, but the policy for handling such edits must be clearly defined in writing. The Standard Operating Procedures (SOPs) must establish a clear distinction between minor corrections and substantive changes, based on risk.
Correcting a simple spelling mistake that does not alter the meaning of a sentence can often follow a simplified documentation process. However, if a change—regardless of its perceived size—could potentially affect patient safety, data integrity, study conduct, or regulatory compliance, it must proceed through the full formal change control workflow. The key is to have a pre-defined, risk-based rule set and to adhere to it consistently, enabling a confident defense of all decisions during an audit.
How Should Change Control Be Handled with External Partners like CROs?
When working with external partners, it is essential to establish clear expectations from the outset and to utilize a single source of truth. A comprehensive Quality Agreement is necessary. This document should detail the entire change control process, define responsibilities, and specify which system will be used by all parties. While the sponsor may delegate tasks, it always retains final responsibility and oversight.
The most effective approach is to have all stakeholders—the internal team, the CRO, and clinical sites—operate within a single, centralized platform. Providing role-based access to the same system eliminates confusion, prevents the circulation of conflicting versions, and maintains one clean, unified audit trail for the entire study. This is how a sponsor can effectively demonstrate oversight to regulators.