A regulatory document management system (RDMS) is a specialized platform designed for authoring, managing, reviewing, approving, and archiving the extensive documentation required for clinical trials and regulatory submissions. Unlike a general-purpose digital filing system, it functions as a controlled environment specifically built to adhere to the stringent requirements of regulatory bodies such as the FDA and EMA.
The system is engineered to enforce compliance with industry standards like ICH Good Clinical Practice (GCP) and regulations governing electronic records, including 21 CFR Part 11.
What Is a Regulatory Document Management System
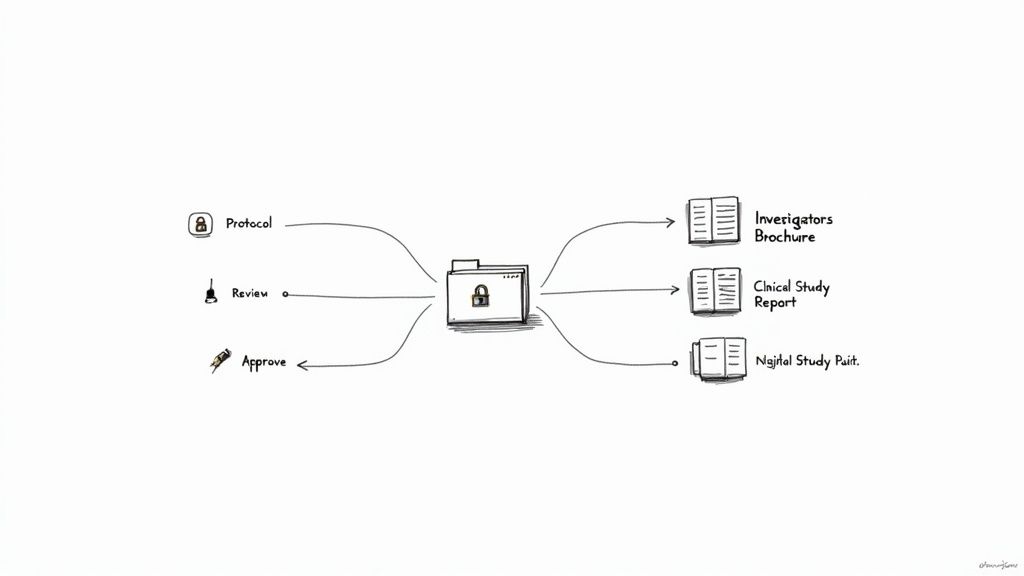
In the context of clinical development, an RDMS is not merely for document storage. It is a system that governs the entire lifecycle of essential documents, from the initial draft of a study protocol to the final, approved Clinical Study Report (CSR).
The system is designed to manage a document as a controlled asset, distinguishing between drafts, reviewed versions, approved final documents, and subsequent amendments. This distinction is critical for operational integrity; it helps prevent the inadvertent use of an outdated protocol, which could impact patient safety and data validity.
A core function of a compliant RDMS is to establish a single source of truth for clinical trial documentation. It centralizes the processes of document authoring, review, and approval, moving them from uncontrolled email chains or shared drives into a structured environment to mitigate version control risks.
This approach creates a complete, auditable history for every document, providing the verifiable evidence required during regulatory inspections by agencies like the FDA or EMA.
Differentiating an RDMS from General Systems
A specialized RDMS should not be confused with a general-purpose document management system (DMS) or file-sharing platforms. While a standard DMS may offer basic version control, an RDMS includes features specifically designed for the life sciences sector.
Key differentiators include:
- Structured Workflows: An RDMS directs documents through predefined, sequential stages for review and approval. It ensures, for example, that a protocol or informed consent form captures all required electronic signatures before the document is finalized and released.
- Granular Access Controls: The system is built to recognize distinct roles within a clinical trial. A medical writer, statistician, and clinical operations lead will have different permissions, ensuring individuals can only access or act upon documents relevant to their function.
- Immutable Audit Trails: A non-negotiable feature, an RDMS generates a secure log of every action performed on a document—including creation, viewing, editing, and approval—with a permanent, computer-generated timestamp. This provides the verifiable record required by auditors.
- Compliance with Industry Standards: These systems are designed to align with regulations like FDA 21 CFR Part 11, which establishes the criteria for trustworthy and reliable electronic records and electronic signatures.
The Operational Role in Clinical Trials
Operationally, the RDMS serves as the central platform for managing all documents that guide and record the conduct of a clinical trial. It is the environment for managing the Investigator's Brochure (IB), the Statistical Analysis Plan (SAP), and the various versions of informed consent forms that arise during a study.
By establishing this controlled environment, a regulatory document management system supports the consistent and compliant authoring, review, and storage of all critical documentation. This structure is foundational to maintaining a state of inspection readiness.
Core Features of a "Regulatory-Grade" Document System
A true RDMS is built upon a foundation of specific controls designed to meet the standards of health authorities like the FDA and EMA. These features are not optional; they are the architectural components that ensure document authenticity, reliability, and traceability from the start of a trial through to final submission.
As clinical trials have grown in complexity, the need for these specialized systems has increased. Market analysis from Grand View Research projects the document management system market will grow from USD 7.68 billion in 2024 to USD 18.17 billion by 2030. This growth is significantly driven by regulated industries seeking compliant solutions. You can explore the document management market trends for more details.
The following sections outline the features that distinguish a basic file-sharing tool from a system suitable for regulatory inspections.
Immutable Audit Trails
The immutable audit trail is the core of a compliant RDMS. It is a secure, computer-generated, time-stamped log that records every interaction with a document, from creation to archival.
This trail provides answers to "who, what, when, and why" for all document activities, specifying:
- Who created the document and when.
- Who edited it, at what time, and often with a reason for the change.
- Who viewed or downloaded the file.
- Who applied an electronic signature for approval.
This functionality directly addresses regulatory requirements like 21 CFR Part 11, which mandates that systems produce complete and accurate records for inspection. An immutable audit trail provides inspectors with a transparent history, demonstrating control and accountability over documentation.
Robust Version Control
Version control is a critical function for preventing operational errors. It is the mechanism that ensures a study coordinator does not use an outdated protocol amendment or an investigator does not reference a superseded Investigator's Brochure.
The use of an incorrect document version at a clinical site can lead to protocol deviations, potentially compromising patient safety and data integrity. Robust version control is designed to prevent such high-impact errors.
A purpose-built RDMS automates version control. When a document is checked out for edits, a new draft version is created (e.g., v0.2). Upon completion of the review and approval cycle, the system designates it as the new effective version (e.g., v2.0) and automatically archives the previous one. This creates a clear document lineage, making it easy to track the evolution of a document without confusion from manual naming conventions.
Granular Access Controls
In a clinical trial, access to documents must be restricted based on role and responsibility. Granular access controls enforce this "need-to-know" principle, which is fundamental to both data security and Good Clinical Practice (GCP).
This feature allows for the configuration of permissions based on an individual's role in the study. For instance:
- A Medical Writer may have edit rights for a Clinical Study Report (CSR) but view-only rights for the study budget.
- A Statistician can view the protocol but has edit permissions only for the Statistical Analysis Plan (SAP).
- A Quality Assurance representative can review and approve documents across multiple functional areas but may not have authoring permissions.
This is more than a security measure; it enforces process. By restricting who can approve a final document or modify a controlled template, the system actively supports adherence to Standard Operating Procedures (SOPs).
Validated Electronic Signatures
Validated electronic signatures are the digital equivalent of handwritten signatures and carry the same legal weight in many jurisdictions. To meet the requirements of 21 CFR Part 11, these signatures must be uniquely linked to an individual, often requiring two-factor authentication such as a unique username and password.
When a user applies an e-signature, the system permanently binds their identity, the date, and the time to that specific document version. This action is recorded in the audit trail, creating an undeniable record of approval. The term "validated" signifies that the system's signature functionality has been formally tested to confirm it is secure and reliable, providing health authorities with confidence in the legitimacy of electronic approvals.
The following table summarizes how these essential RDMS features map to the regulatory principles they support.
Essential RDMS Features Mapped to Regulatory Principles
This table connects key features of a regulatory document management system to the underlying regulatory principles they support, illustrating their direct impact on compliance.
| RDMS Feature | Associated Regulatory Principle (ICH GCP / 21 CFR Part 11) | Operational Impact in Clinical Trials |
|---|---|---|
| Immutable Audit Trail | Accountability & Traceability (21 CFR §11.10(e)): Secure, time-stamped audit trails must be maintained. | Provides inspectors with a defensible, chronological history of every document, demonstrating control and integrity. |
| Robust Version Control | Data Integrity & Document Control (ICH E6 §4.9.4, §8.1): Ensuring only current versions of documents are used. | Prevents use of outdated protocols or forms at clinical sites, reducing protocol deviations and safety risks. |
| Granular Access Controls | Security & Role-Based Access (21 CFR §11.10(d)): Limiting system access to authorized individuals. | Enforces SOPs by restricting actions (e.g., approval) to designated roles, preventing unauthorized changes. |
| Validated e-Signatures | Authenticity & Non-Repudiation (21 CFR §11.50, §11.200): Electronic signatures must be legally binding. | Creates a legally enforceable record of document approval, eliminating the need for printing, signing, and scanning. |
These features collectively create a compliant, controlled environment where the integrity of every critical document is maintained from creation to final archive.
Tracing a Document's Journey Through an RDMS
The function of a regulatory document management system is best understood by observing its role in practice, guiding a critical document from concept to a globally distributed, inspection-ready file.
Consider the development of a clinical study protocol. This process, which can be disorganized when managed via email and shared files, becomes a controlled, compliant workflow within an RDMS.
The process often begins with a controlled template. A medical writer or clinical lead initiates the protocol using a pre-approved, version-controlled template within the system. This ensures that all required sections, structural elements, and standardized language—aligned with guidelines like ICH E6(R3) and internal SOPs—are included from the start.
From Initial Draft to Collaborative Review
Once the initial draft is saved (e.g., Protocol v0.1), the system’s workflow engine initiates the review process. The document is automatically routed to the first set of reviewers, such as the lead statistician and clinical operations manager. The system assigns each individual a task with a clear deadline and sends automated notifications.
As reviewers provide input, the RDMS prevents version fragmentation. Stakeholders add comments and suggested edits directly within the platform's controlled environment, creating a single, centralized location for all feedback associated with that specific draft. The author can then review the feedback, accept or reject changes, and each of these actions is recorded in the audit trail.
The primary function of the RDMS during this stage is to ensure all stakeholders are working from the most current draft. This eliminates a significant source of rework and error common in manual processes.
After the initial feedback is incorporated, the author advances the document to the next draft (e.g., v0.2). This triggers the next workflow step, routing the updated protocol to a broader team that may include regulatory affairs, quality assurance, and pharmacovigilance.
This flow diagram illustrates how these core functions work in concert to protect document integrity.
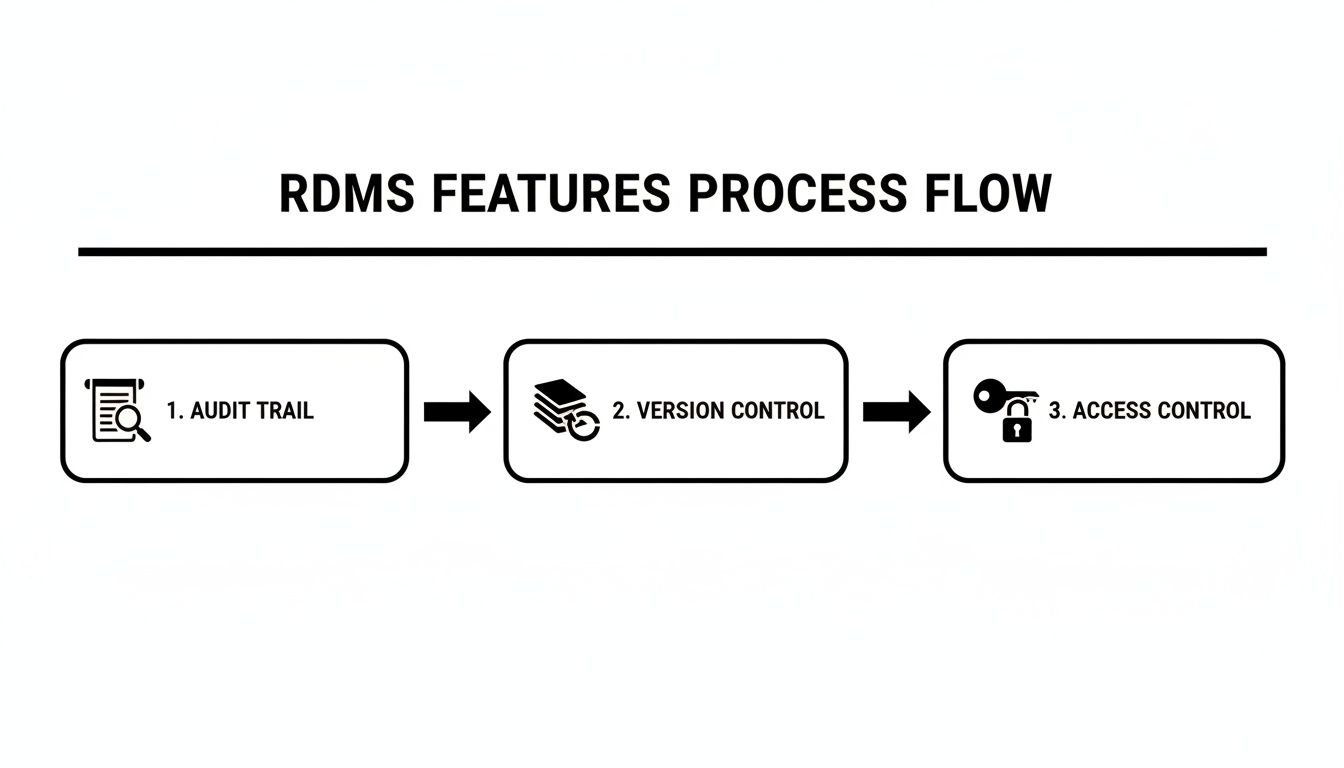
The combination of audit trails, version control, and strict access controls creates a secure and fully traceable lifecycle for every document.
Achieving Final Approval with Electronic Signatures
After several review cycles, the protocol is ready for formal approval (e.g., v0.9). The author submits it for approval, and the RDMS routes it to the designated approvers—such as the Chief Medical Officer or Head of Clinical Development—for their legally binding electronic signatures.
To comply with regulations like 21 CFR Part 11, each approver must authenticate their identity, typically with a unique username and password. Upon signing, the RDMS performs several actions simultaneously:
- It applies a digital, time-stamped signature to the document.
- It promotes the document to its final, effective state (v1.0).
- It renders the file read-only to prevent unauthorized changes.
- It records the entire approval event in the permanent audit trail.
This approved protocol is now the single source of truth. The system can then manage its distribution, making it securely available to authorized personnel at clinical sites, ethics committees, and institutional review boards.
Managing Amendments and Future Versions
A document’s lifecycle continues after initial approval. When a change is required, an authorized user initiates a formal amendment process within the RDMS by "checking out" the effective v1.0. The system automatically creates a new draft for the amendment (e.g., v1.1_draft_0.1).
This new draft undergoes the same rigorous review and approval workflow as the original. Once the amendment is fully approved, it becomes the new effective version (e.g., v2.0), and the system automatically archives the previous version (v1.0). This creates a clear, unbroken history, allowing an auditor to easily trace the entire evolution of the protocol.
This structured process—from template to final version and through every amendment—is applicable to all critical clinical documents, including the Investigator's Brochure (IB) and the Clinical Study Report (CSR). By enforcing a consistent, auditable process, an RDMS ensures that every document is managed with the integrity and control necessary for regulatory submissions and inspection readiness.
Integrating an RDMS with the Broader Clinical Ecosystem
A regulatory document management system operates most effectively when integrated with other clinical trial systems, serving as the central hub for critical documentation. Proper integration creates a single source of truth and breaks down data silos that can cause inefficiency and compliance risk.
When systems are disconnected, teams often resort to manual, duplicative data entry. For example, a protocol finalized in the RDMS might require a manual status update in a separate system. This creates opportunities for human error, which can lead to discrepancies discovered during an audit.
System Interoperability in Clinical Operations
To understand the role of an RDMS, it is useful to see how it interacts with other major platforms in the clinical technology stack. Each system has a distinct purpose, but they often handle the same documents at different stages.
-
Electronic Trial Master File (eTMF): The RDMS is the environment for authoring documents—where protocols, Investigator's Brochures, and ICFs are drafted, reviewed, and approved. The eTMF, in contrast, is the official repository where final documents are archived for inspection. An effective integration ensures that once a document is final-approved in the RDMS, it is automatically transferred to the correct location in the eTMF with all associated metadata preserved.
-
Clinical Trial Management System (CTMS): The CTMS manages the operational aspects of a trial, such as milestone tracking, site monitoring, and investigator payments. When connected to an RDMS, document approvals can automatically trigger updates in the CTMS. For example, the final approval of all essential site documents in the RDMS could automatically change that site's status to "Activated" in the CTMS.
-
Regulatory Information Management (RIM) System: A RIM platform manages the lifecycle of regulatory submissions, from planning and publishing to tracking health authority correspondence. Integrating an RDMS with a RIM system allows final, submission-ready documents to flow directly into the RIM system for assembly into an eCTD, maintaining a clean chain of custody.
Investment in integrated systems is growing as organizations seek to improve trial efficiency and compliance. Market forecasts indicate the increasing importance of this technology; the standalone RIM market was projected to reach USD 2.56 billion in 2025 and is expected to grow to USD 6.25 billion by 2034. This market analysis on regulatory information management systems provides further details.
The Role of Validation and Training
System integration is the first step; maintaining compliance requires two additional non-negotiable activities: system validation and user training.
System validation provides documented evidence that the integrated systems function as intended and meet all applicable regulatory requirements. Without it, there is no verifiable proof that data transferred between an RDMS and an eTMF is accurate and secure.
This process involves rigorous testing of the integrated platform to confirm that automated workflows execute correctly and that audit trails are preserved as data moves between systems.
Finally, effective training is essential for ensuring that teams use the integrated system correctly and follow compliant procedures. This includes clear instructions, ongoing support, and reinforcement of best practices that establish the integrated ecosystem as a reliable source of truth.
How to Select and Manage Your RDMS Effectively
Selecting the right regulatory document management system is a strategic decision that impacts compliance, operational efficiency, and scalability. The evaluation should go beyond a feature comparison to include a thorough assessment of a vendor's experience and the system's suitability for life sciences workflows.
Effective ongoing management is critical for maintaining control and ensuring a constant state of inspection readiness. A well-defined selection and management plan transforms an RDMS from a software tool into an integral component of an organization's quality management system.
Key Selection Criteria for a Life Sciences RDMS
When evaluating systems, certain criteria are non-negotiable for organizations operating in a GxP-regulated environment. These factors distinguish a purpose-built life sciences platform from a generic document management tool.
Key areas for assessment include:
- Life Sciences Experience: The vendor should have demonstrable experience in the pharmaceutical, biotech, or CRO sectors and a deep understanding of clinical trial documentation and regulations like ICH GCP.
- System Validation Package: A reputable vendor should provide a comprehensive validation package. This documentation is essential for supporting internal validation efforts and provides evidence that the system was developed and tested according to GxP standards.
- eCTD Readiness: The system should support the creation of submission-ready documents. This includes features for the specific formatting, metadata, and hyperlinking required for publishing an electronic Common Technical Document (eCTD).
- Scalability: The selected RDMS must be able to scale with the organization's growth in document volume, number of trials, and product portfolio without degradation in performance.
The vendor’s understanding of the regulatory landscape is as important as the software’s technical capabilities. An RDMS should support existing processes rather than forcing adherence to a generic operational model.
Best Practices for Ongoing System Management
After implementation, the objective is to maintain the RDMS as a controlled and reliable source of truth. This requires clear governance and routine maintenance to ensure ongoing compliance.
Two core activities are essential for successful long-term management.
Establishing Clear Governance
Effective governance is built on documented, standardized procedures for system use.
- Document Naming Conventions: Implement a logical and consistent naming convention for all documents. For example, a protocol might follow the structure
[Protocol Number]_[Compound]_[Phase]_[Version]. This simple practice improves findability and reduces confusion. - Metadata Standards: Define mandatory metadata fields for different document types (e.g., study number, document owner, effective date). Consistent metadata enables powerful search capabilities, accurate reporting, and seamless integrations with other systems like an eTMF.
Maintaining Security and Compliance
Regulatory requirements and organizational needs evolve, so system management must be an ongoing activity.
- Periodic User Access Reviews: Conduct regular reviews (e.g., quarterly or semi-annually) of user access rights. This is a fundamental security control that mitigates the risk of unauthorized access, particularly as personnel change roles or leave the organization.
- Staying Informed on Guidelines: Assign responsibility for monitoring updates to regulatory guidelines from agencies like the FDA and EMA. When regulations change, system configurations and internal SOPs may need to be updated to maintain alignment with current expectations.
Achieving Inspection Readiness with an RDMS
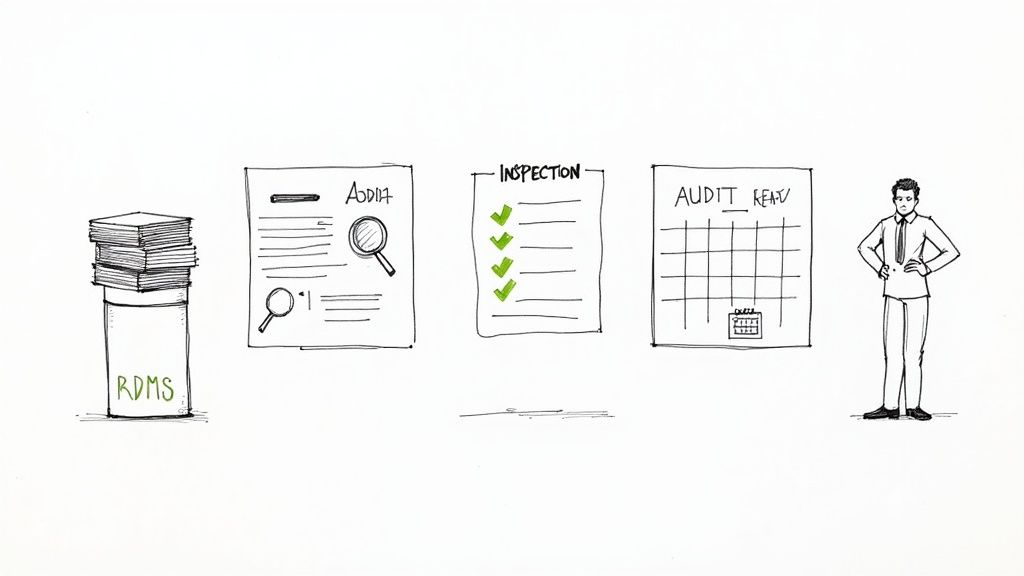
During a regulatory inspection, organizations must be able to produce documents quickly and demonstrate control over their lifecycle. A primary objective of a regulatory document management system is to establish a constant state of inspection readiness, ensuring that all critical documentation is maintained to this standard.
An RDMS serves as a cornerstone of a modern quality management system, transforming document management from a reactive exercise into a proactive, controlled operation. This enables sponsors and CROs to confidently demonstrate complete oversight of their clinical trial documentation.
The Strategic Value of an RDMS
Implementing a purpose-built RDMS is a strategic initiative to enhance operational integrity. It signifies a shift from simple document storage to active lifecycle management of the documents that underpin patient safety and data integrity.
This structured approach provides tangible benefits:
- Demonstrable Control: During an inspection, the complete, immutable history of any requested document, from a protocol amendment to a final CSR, is readily available.
- Reduced Compliance Risk: By automating workflows and enforcing access controls, the system integrates SOPs into daily operations, minimizing human errors that can lead to inspection findings.
- Operational Confidence: Teams can be certain they are always working with the latest, approved version of a document, eliminating version control issues and the risks associated with using outdated information.
An RDMS provides verifiable evidence that an organization not only has established procedures but consistently follows them. This is a primary focus for regulatory inspectors.
By embedding GxP principles into daily workflows, a regulatory document management system makes good documentation practices a routine activity. This foundation of control and traceability is essential for the ultimate goal of developing and delivering safe and effective therapies.
Frequently Asked Questions About RDMS
Understanding how a regulatory document management system fits within an existing clinical technology ecosystem is crucial for operational teams. The following are answers to common questions about these systems.
What is the difference between an RDMS and an eTMF?
This is a common and important question, as both systems manage critical trial documents, but for different purposes.
The RDMS is best understood as the document authoring environment. It is the active, collaborative space where documents such as protocols, Investigator's Brochures, and Clinical Study Reports (CSRs) are drafted, reviewed, and approved. The primary function of the RDMS is to manage the creation and revision lifecycle of a document in a controlled, compliant manner.
The eTMF, conversely, is the official trial archive. Its purpose is to contain the final, approved versions of all essential documents required to reconstruct the trial for a regulatory inspector. Once a document is finalized in the RDMS, it is "published" or transferred to the eTMF. This practice keeps the official record organized (typically according to the TMF Reference Model) and inspection-ready.
Why is system validation necessary?
System validation is a non-negotiable regulatory requirement. It is the process of generating documented evidence that a system functions as intended and meets all applicable GxP regulations.
Without formal validation, regulators will not consider a system compliant for managing GxP-regulated documents. An unvalidated system cannot provide verifiable proof that its audit trails are complete, its version control is reliable, or its electronic signatures are legally binding and secure.
Validation establishes the trustworthiness of the system. It is an ongoing process that provides the objective evidence an inspector will require, making it fundamental to maintaining a state of inspection readiness.
How can an RDMS support global clinical trials?
Global trials introduce additional layers of regulatory and operational complexity, which a well-designed RDMS can help manage.
Key features that support global operations include:
- Custom Workflows: The system can be configured with specific review and approval workflows for different regions. For example, the process for an EMA submission may differ from that for the FDA or Japan's PMDA, and the system can automate these distinct routes.
- Template and Version Management: The system can manage country-specific versions of documents, such as different informed consent forms or regional protocol addenda. This ensures that the correct template is used by the appropriate team.
- Granular Access Control: Access can be precisely controlled based on a user's role and geographic location. This ensures that a clinical team in a specific country only has access to documents relevant to their activities, preventing confusion and supporting regional compliance.
Article created using Outrank