The volume of documentation generated during a clinical trial is substantial, and its organization is a critical operational and regulatory requirement. The DIA Trial Master File (TMF) Reference Model provides a standardized framework for this purpose.
The model is not a regulation or a legally binding requirement. Instead, it is an industry-developed standard that offers a common structure for organizing the documents produced during a clinical trial. It provides a consistent taxonomy, naming convention, and framework that helps sponsors, Contract Research Organizations (CROs), and investigator sites maintain complete, orderly, and inspection-ready TMFs.
Decoding the TMF Reference Model
Prior to the model's establishment, organizations developed proprietary TMF structures. This lack of standardization created operational inefficiencies, particularly during collaborations between sponsors and CROs, mergers and acquisitions, and regulatory inspections. Combining disparate TMF structures was a complex and resource-intensive process prone to error.
In response, a group of industry volunteers collaborated to create a single, logical framework. This framework provides a defined location for all trial-related documentation, from the initial protocol to the final clinical study report, in a predictable and consistent manner.
A Common Language for Clinical Documentation
The DIA TMF Reference Model can be conceptualized as a universal classification system for clinical trial documentation. By establishing a common language and structure, it facilitates clear communication and consistent organization of TMF content across the industry. This shared understanding enhances operational efficiency.
Adopting this structured approach provides several practical benefits:
- Facilitates Collaboration: It enables sponsors, CROs, and technology vendors to exchange and review TMF documents efficiently by working from a common structural blueprint.
- Improves Inspection Processes: Regulatory inspectors familiar with the model can locate required documents more efficiently, allowing them to focus on the content of the documentation rather than its organizational structure.
- Enhances Consistency: The model provides a standard list of document types, known as "artifacts," which helps ensure comprehensive and consistent collection and filing of documentation across studies and sites.
The model is a practical tool derived from industry consensus. It translates the principles of Good Clinical Practice (GCP) regarding "essential documents" into an actionable framework for daily TMF management.
The core attributes of the model are summarized below.
Key Attributes of the DIA TMF Reference Model
| Attribute | Description |
|---|---|
| Standardized Taxonomy | Provides a consistent Zone-Section-Artifact hierarchy for all TMF documents. |
| Industry-Driven | Developed and maintained by a volunteer group of industry professionals, not a regulatory body. |
| Not a Regulation | It is a best-practice recommendation that offers a method to support regulatory compliance. |
| Comprehensive | Aims to include a placeholder for every possible document generated during a clinical trial. |
| Technology Agnostic | The model can be applied to both paper-based and electronic TMF (eTMF) systems. |
| Version Controlled | It is periodically updated to reflect changes in regulations and industry practices. |
The model provides a clear organizational structure based on regulatory requirements and international guidelines. Understanding the principles of ICH GCP is fundamental to appreciating the regulatory context that underpins the TMF and the model's structure.
A Look Back: The Need for TMF Standardization
To understand the significance of the DIA Trial Master File Reference Model, it is helpful to consider the operational environment that preceded it. The absence of a universal standard for TMF organization created significant operational challenges and regulatory risks.
Previously, each sponsor, CRO, and vendor developed its own TMF structure. Consequently, a core document such as an Investigator's Brochure might be filed in different locations with varying nomenclature depending on the organization's system. This lack of consistency complicated collaboration, mergers, and regulatory inspections.
The Turning Point: Establishing a Common Framework
These inconsistencies resulted in increased time and resource expenditure. Transferring a TMF from a CRO to a sponsor, for example, often required a manual re-indexing and refiling of thousands of documents. This process was inefficient and unsustainable.
The solution emerged from industry collaboration. On March 23, 2009, a group of approximately 20 TMF, regulatory, and quality assurance professionals convened to address this challenge. Working under the auspices of the Drug Information Association (DIA), their objective was to create a standard TMF structure that aligned with ICH GCP and could be adopted industry-wide. A detailed review of the TMF Reference Model's history provides further context on its development.
Key Milestones in Standardization
The initial version provided a solid foundation, but the model's utility lies in its adaptability. It is a dynamic standard that evolves based on feedback from its users.
Significant updates over the years include:
- Version 2.0 (2012): This version introduced process-based metadata, enabling teams to track documents in alignment with trial workflows. The model's scope was expanded to include the Investigator Site File (ISF), medical device trials, and Investigator-Initiated Studies (IIS).
- Version 3.0 (2015): This release focused on enhancing the model's practicality. It refined artifact definitions, reorganized some Zones for a more logical flow, and introduced the concept of sub-artifacts. This provided teams with greater flexibility to group related documents under a parent artifact.
- Version 3.2.0 (2020): In response to user feedback, this version added over 600 optional sub-artifacts, allowing organizations to implement more granular filing structures while maintaining adherence to the core standard.
The model has evolved from a simple filing index into a dynamic operational tool. Each version has increased its flexibility to accommodate different trial types and organizational structures while preserving the fundamental value of standardization.
A New Home at CDISC
In June 2022, stewardship of the model was transferred to the Clinical Data Interchange Standards Consortium (CDISC). This strategic move integrates the TMF Reference Model with other major clinical data standards managed by CDISC.
This transition supports the model's future development, ensuring its evolution is harmonized with other critical standards like SDTM and CDASH. Bringing TMF and data standards under a single governance structure promotes interoperability across the clinical trial lifecycle. This move reinforces the TMF's role as a strategic asset and ensures the DIA Trial Master File Reference Model will continue to evolve in line with industry needs.
Understanding the Core Structure of Zones and Artifacts
To effectively use the DIA TMF Reference Model, it is essential to understand its logical structure. It is a three-tiered hierarchy designed to provide a specific location for every document, creating a predictable and consistent filing system for any clinical trial.
The three key structural components are:
- Zones: The highest level, grouping documents by general function or a major phase of the trial.
- Sections: Sub-categories within each Zone that create more focused groupings around specific processes.
- Artifacts: The most granular level, representing a specific type of document, each with a unique identification number.
This layered approach transforms a TMF from a simple repository into a dynamic system that reflects the clinical trial lifecycle. It serves as a standardized roadmap that sponsors, CROs, and regulators can use to locate documents, regardless of the specific eTMF system in use.
The 11 Foundational Zones
The DIA TMF Reference Model is organized into 11 core Zones. Each Zone functions as a major organizational category for the clinical trial, containing documents related to a specific operational area. This logical grouping facilitates document retrieval, management, and review.
For example, Zone 01 (Trial Management) contains high-level documents such as the TMF Plan and various oversight plans. Zone 05 (Investigator Site Management) includes all documentation related to investigator sites, from selection and initiation through monitoring and close-out. Familiarity with the scope of each Zone is the first step toward proficient use of the model.
From Sections to Specific Artifacts
Each Zone is further subdivided into multiple Sections, which provide another layer of organization. If a Zone is a chapter, a Section is a specific heading within that chapter. For example, within Zone 05 (Site Management), Section 05.02 pertains to Site Initiation, while Section 05.03 covers Site Monitoring.
The most detailed organizational level is the Artifact. An artifact is not the document itself but rather the placeholder for a specific type of document, identified by a unique number.
Consider the Informed Consent Form template, which is assigned artifact number 05.04.01. The breakdown is as follows:
- 05 indicates it belongs in Zone 05 (Site Management).
- 04 places it within Section 05.04 (Informed Consent).
- 01 is the unique identifier for that specific artifact (Informed Consent Form Template).
This numbering system creates a universal reference for TMF documents that is understood by all members of the study team.
The following image illustrates the progression from unstructured TMFs to a standardized model.
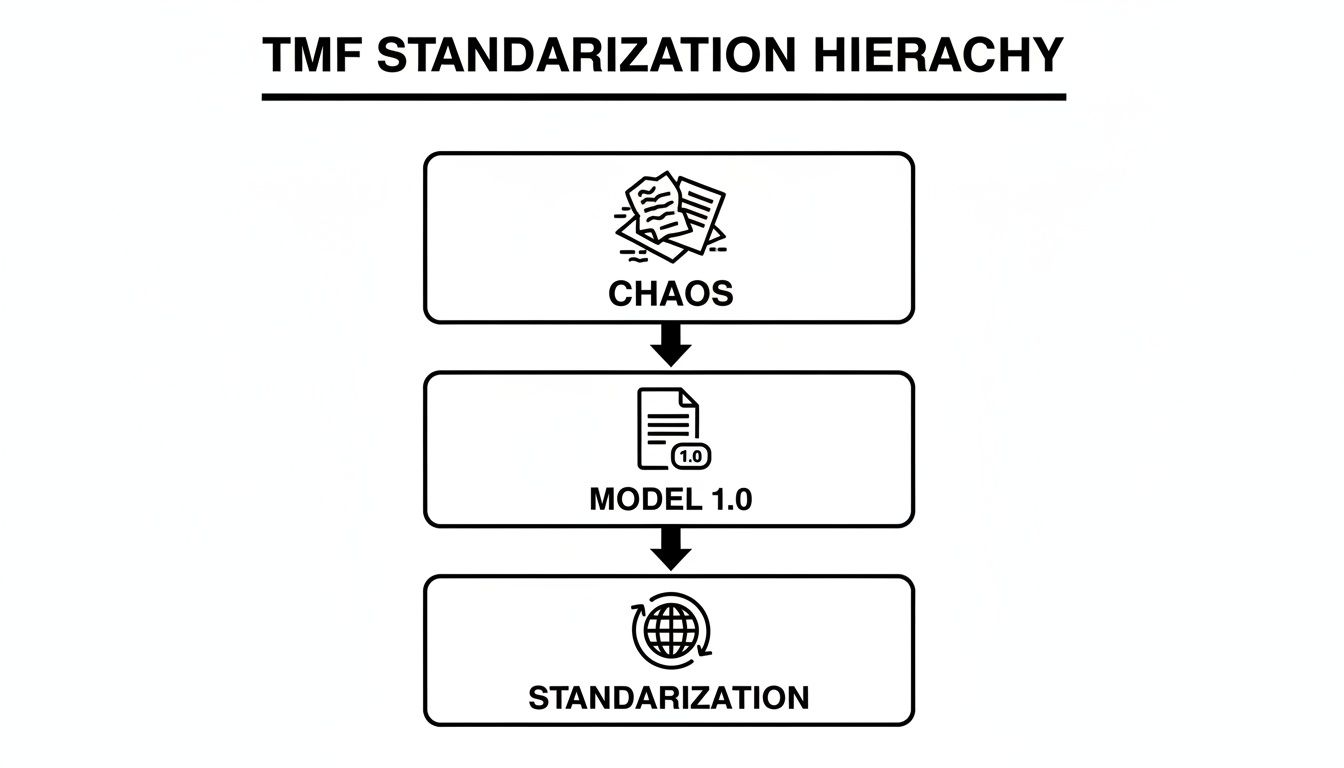
The image shows a clear progression from a chaotic state to a globally recognized standard, addressing the industry's need for improved consistency and quality.
Distinguishing the Artifact from the File
A common point of confusion for teams new to the model is the distinction between an "artifact" and the actual document file. An artifact is the definition or placeholder within the model—analogous to a pre-printed label on a folder. The actual electronic file, such as a PDF of the signed protocol, is the content placed within that folder.
The DIA TMF Reference Model provides the "what" and "where" for trial documents. The artifact defines what the document is (e.g., Protocol Signature Page), and its Zone/Section specifies where it should be filed. The electronic file itself is the evidence that fulfills that requirement.
Understanding this distinction is critical when configuring an eTMF system or performing quality control. The system is configured with the standard artifact list, and the team's responsibility is to upload the correct files and map them to the appropriate artifact placeholder. This ensures the TMF is populated correctly.
The table below provides an example of the hierarchy for a common document.
Example of DIA TMF Reference Model Hierarchy
| Hierarchical Level | Example Component | Description |
|---|---|---|
| Zone | 02 – Central Trial Documents | A high-level grouping for core documents applicable to the entire trial. |
| Section | 02.01 – Protocol and Amendments | A sub-category within Zone 02 for the protocol and related documents. |
| Artifact | 02.01.03 – Protocol Signature Page | The specific placeholder for the signed-off version of the protocol's signature page. |
As shown, the structure provides a logical, top-down path to file and retrieve any essential document.
The Critical Role of Metadata
The Zone-Section-Artifact structure is supported by metadata. Metadata, or "data about data," provides the context that makes each document searchable and useful. While the artifact number identifies what a document is, metadata provides additional information about it.
Common metadata fields include:
- Document Status: e.g., Draft, Final, or Superseded.
- Country: The country to which the document applies.
- Site: The clinical site to which a document, such as a delegation log, belongs.
- Approval Date: The date the final version was approved.
In an eTMF system, standardized metadata enables powerful searching, filtering, and reporting capabilities. For example, a study manager could generate a report of all "Final" protocols across all participating countries. This level of control is fundamental for maintaining TMF health and inspection readiness.
How to Implement the Model in Your eTMF System
Implementing the DIA TMF Reference Model within an electronic Trial Master File (eTMF) system requires a structured approach. The model serves as a blueprint, but its successful implementation depends on careful configuration tailored to an organization's specific needs.
This initial setup is a foundational step that transforms an eTMF from a simple digital repository into a structured and compliant management tool.
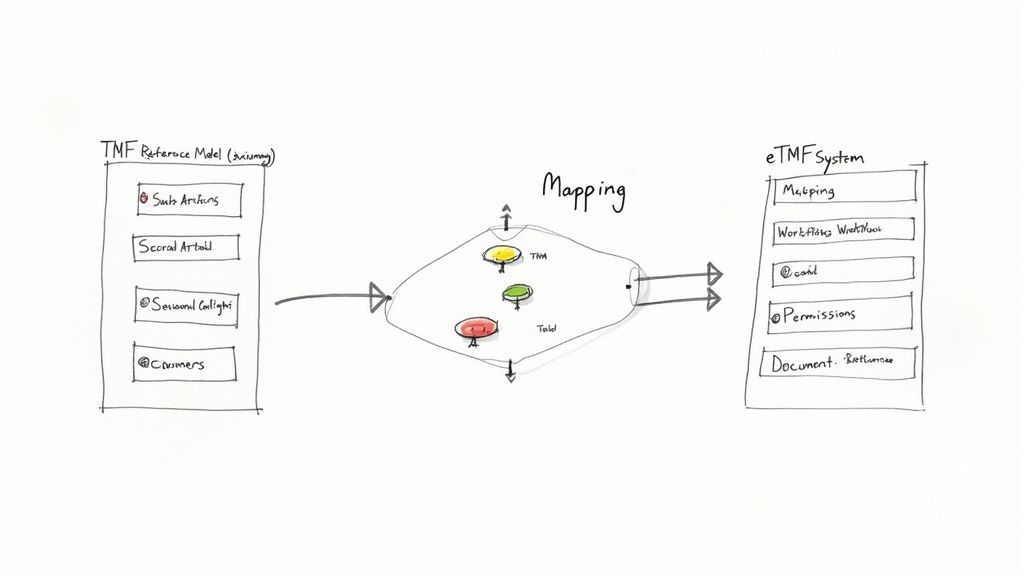
The process begins with a comprehensive mapping exercise. A cross-functional team, including representatives from clinical operations, regulatory affairs, and quality assurance, should review the entire DIA TMF Reference Model artifact list. The model is intentionally comprehensive, so the team's first task is to determine which artifacts are applicable to the organization's studies.
Omitting this step can result in a cluttered eTMF with empty placeholders for documents that will never be generated. Such clutter can negatively impact completeness metrics and complicate TMF management.
Mapping the Model to Your Processes
The mapping process should be deliberate and well-documented. A key consideration is how to manage documents that are not included in the standard model, such as study-specific, country-specific, or internal company documents.
Several strategies can be employed to handle these unique documents:
- Use the ".99" Artifacts: The model includes generic placeholders (e.g., artifacts ending in .99) for this purpose, where custom documents can be assigned.
- Create Sub-artifacts: If the eTMF platform supports it, custom sub-artifacts can be created under the most logically relevant existing artifact. For instance, a unique Spanish regulatory submission form could be a sub-artifact under the main regulatory submission artifact.
- Document Everything in the TMF Plan: All decisions regarding document locations, particularly for non-standard documents, must be clearly defined in the TMF Plan or a dedicated TMF Index.
The TMF Plan serves as the single source of truth, explaining how and why the TMF for a particular study is structured. It is one of the first documents requested during a regulatory inspection.
Detailed planning is essential. The industry's adoption of eTMF systems increased from 13% in 2014 to 65% by 2018. However, data migration projects can be subject to delays and cost overruns, highlighting the importance of meticulous planning. This planning is necessary to comply with evolving regulations, such as the EU Clinical Trials Regulation, which requires the TMF to be maintained in real-time. More information is available on the official CDISC TMF Reference Model page.
Configuring the eTMF Platform
Once mapping decisions are documented in the TMF Plan, the next phase is to configure the eTMF platform. This involves translating the theoretical structure into a functional system with appropriate settings, workflows, and permissions.
Key configuration steps include:
- Build the Taxonomy: Set up the Zone, Section, and Artifact hierarchy within the eTMF to match the finalized TMF index.
- Define Metadata: Configure metadata fields for each artifact, specifying which are required (e.g., country, site) and which are optional to ensure consistent documentation.
- Set User Permissions: Establish role-based access controls to protect data integrity, ensuring team members can only view, upload, or approve documents relevant to their roles.
- Create Workflows: Develop automated workflows for document review, quality control (QC), and approval that align with Standard Operating Procedures (SOPs) and integrate compliance into daily operations.
Proper configuration is what enables an electronic trial master file software platform to function effectively. A well-configured system not only enforces the structure of the DIA TMF Reference Model but also helps streamline workflows, improve oversight, and maintain a state of continuous inspection readiness.
TMF Governance and Maintenance: From Setup to Inspection Readiness
Adopting the DIA TMF Reference Model is an important first step, but ongoing governance and maintenance are essential for ensuring the long-term integrity of the Trial Master File. TMF management should be viewed as a continuous process of oversight that keeps the TMF complete, accurate, and ready for inspection at all times.
A robust governance framework is built on clearly defined roles and responsibilities. All study team members, from Clinical Research Associates (CRAs) to Project Managers, must understand their specific duties regarding TMF documentation. When roles are clear, accountability for filing, reviewing, and approving trial artifacts becomes an integral part of the workflow.
The TMF Plan: Your Study's Single Source of Truth
The TMF Plan is the cornerstone of the TMF governance strategy. It is the single source of truth that outlines all documentation-related processes for a specific study. This plan should serve as the definitive guide, detailing the who, what, where, when, and how of TMF management.
An effective TMF Plan specifies:
- Study-Specific Index: A complete, tailored list of all documents expected for the trial, including any modifications or additions to the standard DIA TMF Reference Model.
- Ownership and Responsibilities: Clear assignment of individuals or roles responsible for creating, filing, and performing quality control (QC) on each document type.
- Filing Timelines: Defined expectations for when documents must be filed in the TMF after finalization, which is critical for demonstrating contemporaneous filing.
- System and Location Details: Specific information on where all TMF components are located, which is especially important for hybrid TMFs or studies involving multiple vendors with separate systems.
The TMF Plan is a living document that must be reviewed and updated in response to protocol amendments, the addition of new vendors, or changes in internal processes.
Monitoring TMF Health with Key Metrics
Proactive TMF maintenance involves tracking key performance indicators, often referred to as TMF health metrics. These metrics provide an objective assessment of the TMF's condition, helping to identify potential issues before they become significant compliance risks. The three pillars of TMF health are:
- Completeness: The percentage of expected documents that are present in the TMF. This metric is a primary indicator of potential missing documentation.
- Timeliness: The speed at which documents are filed after finalization. This directly measures adherence to contemporaneous filing requirements.
- Quality: The correctness of filed documents, including checks for legibility, accuracy, and proper location and metadata.
As stated in ICH GCP E6(R2), sponsors are required to ensure the TMF is "complete, and the documents… should be filed in a timely manner." TMF health metrics provide the tangible evidence needed to demonstrate consistent adherence to this expectation.
These metrics should be reviewed regularly, for example, during monthly TMF review meetings. Consistent monitoring not only protects the integrity of the TMF but also fosters a culture of proactive compliance. A modern regulatory document management system can automate the tracking of these critical metrics.
Managing Change and Staying Aligned
Clinical trials are dynamic, as is the DIA TMF Reference Model. The model is updated periodically to reflect new regulations and evolving best practices. An effective governance plan must include a clear process for managing these changes.
When a new version of the Reference Model is released, its impact on the current TMF setup must be assessed. This involves reviewing new or modified artifacts and determining how to incorporate them into ongoing and future studies. Similarly, a formal change management process should be in place for internal changes, such as new SOPs or technology. Documenting these decisions and training study teams are critical steps for maintaining a consistent and compliant TMF.
Strategic Value of a Standardized TMF
The value of the DIA Trial Master File Reference Model extends beyond its organizational structure; its adoption provides strategic advantages for the entire clinical trial operation.
Implementing the model integrates the TMF as an active component of an organization's quality management system. It demonstrates a commitment to operational excellence, data integrity, and patient safety to both internal teams and regulatory authorities.
The model's primary contribution is its ability to facilitate collaboration. When sponsors, CROs, and technology vendors all use the same framework, operational processes become more efficient. This shared language streamlines activities such as TMF transfers and oversight between partners, reducing the potential for misunderstandings.
Improved Collaboration and Inspection Readiness
A standardized TMF structure directly enhances inspection readiness. From a regulatory inspector's perspective, a familiar TMF layout allows them to focus on the substance of the trial documentation rather than deciphering a unique filing system.
This clarity and predictability can increase confidence with regulatory authorities, contributing to more efficient and successful audits.
Adopting the DIA TMF Reference Model is a strategic decision to align with global best practices, mitigate regulatory risk, and streamline the path from clinical development to regulatory approval.
Consistent use of a framework like the DIA TMF Reference Model is essential for the industry. It provides the transparent and universally understood documentation backbone required for predictable, data-driven clinical trials.
As studies grow in complexity and global scale, a shared standard becomes a fundamental requirement for success. The model is a key component in building a more connected and efficient clinical research ecosystem.
Frequently Asked Questions About the TMF Reference Model
This section addresses common questions that arise when teams begin working with the DIA TMF Reference Model.
Is The DIA TMF Reference Model Required by Law?
No, the DIA TMF Reference Model is not a regulation or a law. It is a best-practice framework and an industry standard developed by clinical trial professionals.
Regulatory bodies such as the FDA and EMA do not mandate its use. However, they generally view its adoption favorably because a TMF structured according to the model is often more complete, logical, and inspection-ready, which aligns with ICH GCP principles. While its use is voluntary, it is a widely recognized best practice.
What Do We Do with Documents That Aren't in The Model?
It is common for a trial to generate documents not explicitly listed in the model. The recommended approach is to map these documents to the most logical location within the existing structure. This may involve placing a document under an existing artifact with a similar purpose or using a designated placeholder, such as one of the ".99 Other" artifacts.
The critical step is to document this decision. The study-specific TMF Plan (or Index) should clearly state where the unique document was filed and provide the rationale. This creates a transparent roadmap for team members and regulatory inspectors.
Can We Modify The TMF Reference Model?
Yes, the model is designed to be flexible and can be adapted to meet an organization's specific needs. It is not intended to be a rigid, unchangeable structure.
Common modifications include:
- Deactivating non-applicable artifacts: Optional artifacts that do not apply to a specific study can be deactivated.
- Adding sub-artifacts: Organizations can create custom sub-artifacts to achieve greater granularity in certain areas.
- Defining custom metadata: Additional metadata fields can be created to track specific information not included in the standard model.
The key is to maintain the integrity of the core Zone and Section structure to ensure industry-wide consistency. All modifications should be controlled, documented in SOPs and the TMF Plan, and communicated to the relevant teams to ensure the TMF remains consistent and defensible.
Article created using Outrank