A clinical study report (CSR) template serves as the standardized framework for authoring the comprehensive account of a clinical trial for regulatory authorities. This structured blueprint, designed in accordance with guidelines like ICH E3, ensures that all critical information is presented logically and consistently for review by agencies such as the FDA and EMA.
The Role of a CSR Template in Clinical Operations
A Clinical Study Report (CSR) is an integrated, exhaustive document detailing a clinical trial's complete lifecycle, from its rationale and design to its conduct, analysis, and results. A well-designed clinical study report template provides the foundational structure for organizing this complex information methodically.
The template functions as a procedural guide for medical writers and clinical teams, ensuring that all required sections are addressed. This standardization mitigates the risk of omissions that could lead to regulatory queries and submission delays. It also promotes consistency across multiple studies within a sponsor’s portfolio, streamlining both internal review and external regulatory assessment.
Distinguishing Key Document Stages
Precise terminology is essential in regulatory documentation. Understanding the distinction between the stages of a CSR's development is fundamental to the process:
- Template: The foundational shell document. It contains the prescribed section headings, subheadings, and instructional text based on regulatory guidelines like ICH E3 but includes no study-specific data.
- Draft: When study-specific information from the protocol, statistical analysis plan (SAP), and trial results is incorporated into the template, it becomes a draft CSR. This version undergoes iterative review and revision by the multidisciplinary study team.
- Final CSR: Following the incorporation of all stakeholder feedback and final sponsor approval, the document is finalized. This is the official version submitted to regulatory authorities as part of a marketing application or other regulatory filing.
A Cornerstone of Regulatory Documentation
The adoption of the ICH E3 guideline in 1996 established the fundamental structure for the CSR that remains the global standard. Standardized CSR templates are direct operational implementations of this guideline.
A CSR template is a critical component of a sound regulatory documentation strategy. It provides a systematic framework for presenting clinical evidence, ensuring the trial’s narrative is communicated with scientific rigor, transparency, and adherence to the format expected by regulatory reviewers.
The table below outlines the essential components of a standard template compliant with ICH E3.
Key Components of a Standard CSR Template
| Component | Purpose and Scope |
|---|---|
| Title Page & Synopsis | Provides a high-level overview, including the study title, protocol number, investigators, and a concise summary of the objectives, methods, and results. |
| Table of Contents | A navigational guide to the entire document, listing all sections, tables, figures, and appendices. |
| Ethics | Details the Institutional Review Board (IRB) or Independent Ethics Committee (IEC) approvals and confirms the study was conducted ethically. |
| Investigators & Study Admin | Lists all key personnel, their roles, and the administrative structure of the study. |
| Introduction | Sets the context for the study, explaining the rationale and scientific background for the trial. |
| Study Objectives | Clearly states the primary and secondary objectives the study was designed to investigate. |
| Investigational Plan | The core "how-to" section, describing the study design, patient population, treatments, and methods for data collection and analysis. |
| Study Patients | Provides a detailed account of patient disposition, demographics, and other baseline characteristics. |
| Efficacy Evaluation | Presents the analysis and results related to the study's primary and secondary efficacy endpoints. |
| Safety Evaluation | Details all safety findings, including adverse events, lab results, and overall patient safety assessments. |
| Discussion & Conclusions | Interprets the efficacy and safety results, discusses their clinical significance, and provides overall conclusions. |
| Appendices | Contains supplementary materials like the protocol, sample case report forms (CRFs), statistical details, and investigator information. |
Each of these components is critical for building a comprehensive and defensible report for regulatory review.
The template ensures the final CSR aligns with other key trial documents, forming a cohesive part of the larger submission package and maintaining document integrity within the Trial Master File (TMF). The relationship between these documents is defined in frameworks such as the DIA TMF reference model.
Deconstructing the ICH E3 Guideline for CSR Templates
The International Council for Harmonisation (ICH) E3 guideline is the universally accepted standard for the structure and content of a Clinical Study Report (CSR). A clinical study report template based on this guideline ensures the final document is structured, complete, and organized in the format expected by reviewers at agencies like the FDA and EMA.
The guideline methodically organizes trial data into 16 distinct sections. Each section serves a specific function, collectively building a transparent and comprehensive account of the study's design, execution, and outcomes. Adherence to this structure is a fundamental requirement for regulatory submissions.
This progression from a standardized blueprint to a final, submission-ready document is a core principle of regulatory documentation.
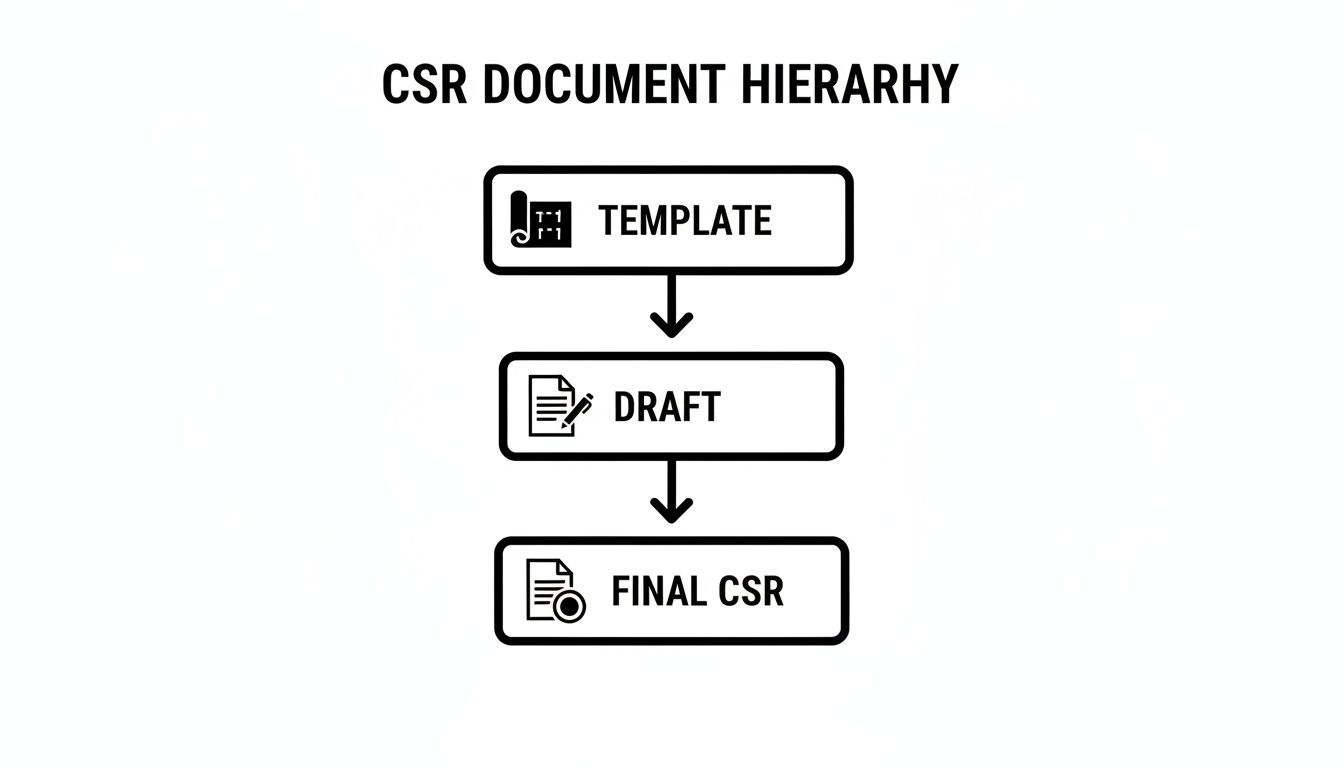
The template provides the structural framework, which guides the authoring of the draft CSR. This draft is then refined through review cycles into the final, compliant document.
Mapping the 16 Core Sections of ICH E3
Familiarity with the ICH E3 structure is the first step toward preparing a compliant CSR. Each of the 16 sections builds upon the last, creating a cohesive and scientifically rigorous account of the trial. An effective template will include placeholders and instructional text for each mandated component.
The key sections a template must include are:
-
Title Page: This section contains essential identifiers: study title, protocol number, development phase, sponsor information, and the report date.
-
Synopsis: This is a standalone summary (typically limited to three pages) covering the study's objectives, design, methods, and key results. It provides reviewers with a high-level overview of the trial.
-
Table of Contents: This serves as a detailed roadmap, listing all sections, tables, figures, and appendices to facilitate navigation.
-
List of Abbreviations and Definitions: A glossary defining all abbreviations and technical terms used in the report, ensuring clarity and consistency.
-
Ethics: This section documents that the study was conducted in accordance with ethical principles. It must detail the Institutional Review Board (IRB) or Independent Ethics Committee (IEC) that approved the study and describe the informed consent process.
-
Investigators and Study Administrative Structure: This section lists key personnel, including the principal investigators and coordinating investigators, and outlines the trial's administrative framework.
-
Introduction: This section provides the scientific context for the study, including background on the investigational product and the clinical condition under investigation.
-
Study Objectives: A clear and concise statement of the primary and secondary objectives the study was designed to address.
The Core of the Report: Study Conduct and Results
The subsequent sections contain the detailed substance of the report, describing the trial's methodology and presenting the collected data.
-
Section 9 – Investigational Plan: This is a comprehensive description of the study's methodology. It details the overall study design, treatment arms, patient selection criteria (inclusion/exclusion), and all efficacy and safety assessments. It also describes the statistical methods outlined in the Statistical Analysis Plan (SAP) and documents any deviations from the original protocol.
-
Section 10 – Study Patients: This section provides a complete accounting of the patient population, including patient disposition (e.g., completion/withdrawal status), demographic data, and other baseline characteristics.
-
Section 11 – Efficacy Evaluation: This section presents the results for the study's primary and secondary efficacy endpoints. It relies heavily on data displays, such as tables, figures, and listings, to support the narrative.
-
Section 12 – Safety Evaluation: This is a thorough analysis of all safety data. It includes the extent of patient exposure to the investigational product, a summary of adverse events (AEs), serious adverse events (SAEs), and relevant laboratory findings.
Concluding the Narrative and Providing Supporting Documents
The final sections of the CSR template focus on interpretation and provide access to all supporting documentation, ensuring the report is fully auditable.
A well-structured template guides the author to not only present data but to construct a coherent scientific argument. The Discussion and Conclusion sections are where the evidence comes together to tell the final story of the trial.
-
Section 13 – Discussion and Overall Conclusions: This section synthesizes the efficacy and safety results, discusses their clinical significance in the context of other relevant data, and provides an overall benefit-risk assessment.
-
Section 14 – Tables, Figures, and Graphs Referred to but Not Included in the Text: A dedicated section for large data displays that are referenced in the main body but are too extensive to be embedded directly.
-
Section 15 – List of References: A standard bibliography citing all publications and documents mentioned in the report.
-
Section 16 – Appendices: This is the repository for essential source documents, including the study protocol, a sample Case Report Form (CRF), the statistical analysis plan, and investigator information. This makes the CSR a complete, self-contained record.
Operationalizing the CSR Template: A Practical Workflow
A clinical study report template is more than a static document; it is a tool that must be integrated into clinical operations. Transforming a template into a final CSR requires a defined workflow, clear role delineation, and appropriate systems to manage the process from first draft to final submission.
This process involves orchestrating a multidisciplinary team, ensuring data consistency across numerous source documents, and maintaining a complete audit trail of all changes. The objective is a collaborative process that produces an accurate CSR efficiently and without last-minute complications.
Defining Roles and Responsibilities
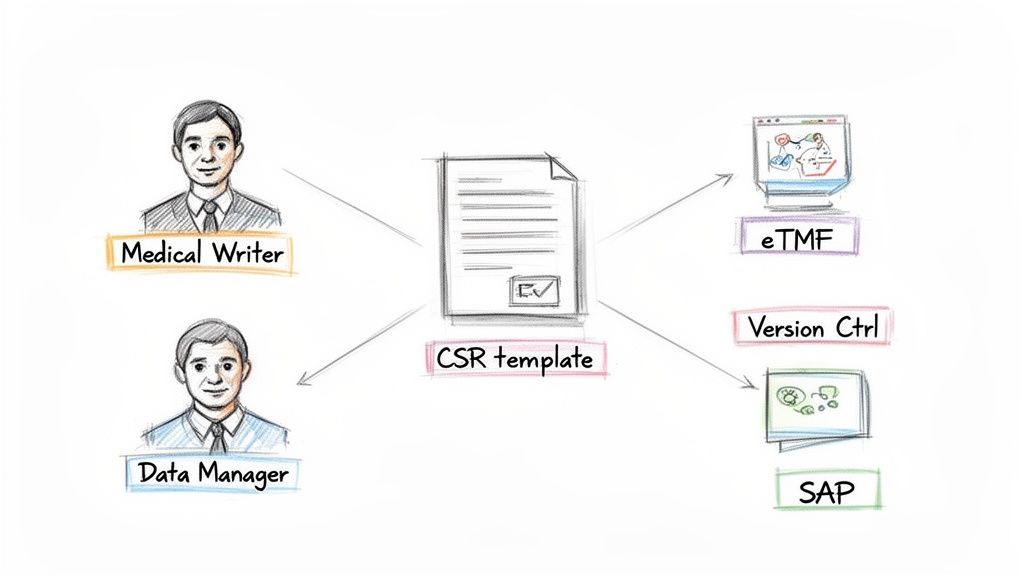
A CSR is developed by a team of specialists, and clearly defined roles are essential to prevent bottlenecks and confusion. A typical CSR team includes several key roles.
- Medical Writers typically lead the drafting of the narrative, integrating data from various sources to ensure the final report presents a clear and compliant account.
- Biostatisticians are responsible for providing all tables, listings, and figures (TLFs) and for authoring or reviewing the statistical sections to ensure their accuracy and soundness.
- Data Managers provide the clean, locked clinical database and offer critical input on data collection and management procedures.
- Clinical Scientists/Physicians provide the clinical context, interpreting the efficacy and safety data and contributing to the discussion and conclusions sections.
This collaborative approach ensures that all scientific, statistical, and clinical aspects are addressed with appropriate expertise.
Version Control and Review Cycles
Without robust version control, a CSR document can become difficult to manage, particularly with multiple authors and reviewers contributing simultaneously. A systematic approach is non-negotiable.
A CSR is a living document during its development. An effective workflow requires a controlled environment where every edit, comment, and approval is tracked, creating a transparent history of the document's evolution from an empty template to a final submission.
A regulatory document management system is designed for such complex workflows. These platforms provide controlled access, automated versioning, streamlined comment resolution, and electronic signatures to maintain order and compliance. To learn more about these tools, you can explore how a regulatory document management system functions.
Linking to Source Documents for Consistency
The CSR is derived from a library of other key documents, and its credibility depends on its consistency with them. A robust workflow must include checks to ensure alignment.
The most important source documents include:
- The Study Protocol: The methods sections of the CSR must accurately reflect the final approved protocol and any subsequent amendments. Any deviations must be documented and justified.
- The Statistical Analysis Plan (SAP): The statistical methods and results presented in the CSR must directly correspond to the analyses specified in the SAP.
- Investigator’s Brochure (IB): All safety information and background on the investigational product must align with the current version of the IB.
Using an eTMF (electronic Trial Master File) or a similar centralized platform is an operational best practice for managing these dependencies. When all key documents reside in a single, controlled repository, the team can easily cross-reference information and trace data back to its source. This reduces the risk of inconsistencies that can attract regulatory scrutiny.
Navigating Common Pitfalls in CSR Preparation
Even with a well-designed template, the process of preparing a Clinical Study Report (CSR) presents numerous challenges. The template provides the structure, but the quality of the final report depends on rigorous execution and the avoidance of common errors that can attract regulatory scrutiny. Awareness of these potential pitfalls is key to producing a clear, scientifically sound CSR that accurately represents the trial.
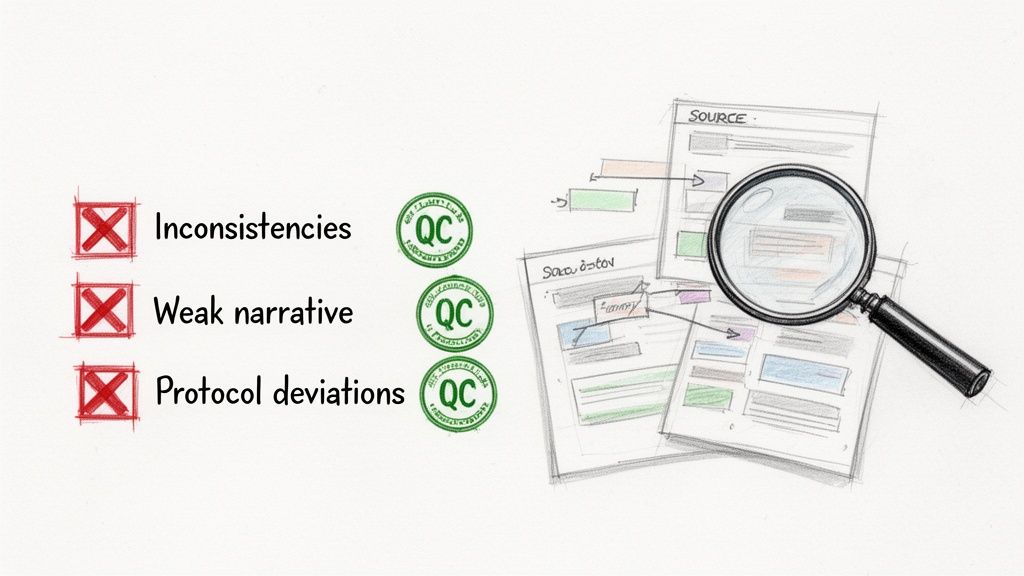
Successful CSR preparation requires a deep understanding of how different data sources interrelate and a commitment to clear scientific communication. Common issues include inconsistencies between documents, a weak scientific narrative, and inadequate reporting of study conduct.
Inconsistent Information Across Source Documents
One of the most critical and common errors is a lack of alignment between the CSR and its source documents, such as the protocol, the Statistical Analysis Plan (SAP), or the clinical database. For example, a reviewer may note that patient disposition numbers in the CSR do not match the final database lock, or that the statistical methods described deviate from the SAP without justification.
Such discrepancies can undermine the credibility of the entire report. They suggest inadequate internal quality control and can trigger extensive queries from regulatory agencies, potentially delaying the review process.
- Best Practice: Establish a formal Quality Control (QC) process where reviewers, independent of the writing team, perform a line-by-line check of key data points, tables, and narrative text against the locked database, SAP, and final protocol.
Insufficient Narrative in Efficacy and Safety Sections
Presenting tables and figures without a clear, interpretive narrative is a significant deficiency. The CSR must explain what the efficacy and safety data mean. The narrative should guide the reviewer through the results, highlighting the most clinically relevant findings.
A report that is merely a "data dump" forces regulators to draw their own conclusions. The goal is to present a complete and coherent scientific argument.
The narrative is the scientific soul of the CSR. It transforms raw data into a coherent story that explains the trial's outcomes, preemptively addresses potential questions, and builds a strong case for the product's benefit-risk profile.
- Best Practice: Develop a narrative strategy and agree upon the key messages with the multidisciplinary team before writing begins. This collaborative planning between medical writers, clinicians, and biostatisticians ensures the narrative is consistent, scientifically robust, and fully supported by the data.
Poorly Explained Protocol Deviations
No clinical trial is executed perfectly; protocol deviations are inevitable. However, failing to properly document, categorize, and explain them is a major deficiency. A CSR that provides only a superficial account of deviations or fails to assess their impact on study integrity can suggest poor trial oversight or a lack of transparency.
This is a significant concern for regulators, as it can call into question the validity of the study results.
- Best Practice: Maintain a detailed, contemporaneous log of all protocol deviations throughout the study. In the CSR, describe each significant deviation and provide a thoughtful analysis of its potential impact on the efficacy and safety data. This proactive approach demonstrates transparency and rigorous study management.
A well-managed documentation process is foundational to all of these practices and is a critical part of maintaining an audit-ready trial master file. For more information, see our guide to electronic trial master file software.
The following table summarizes how to convert these common pitfalls into best practices.
CSR Template Pitfalls vs Best Practices
| Common Pitfall | Recommended Best Practice |
|---|---|
| Data Mismatches: Patient counts, statistical methods, or endpoints in the CSR don’t align with the protocol, SAP, or clinical database. | Dedicated QC Team: Implement a formal, independent QC review to verify all key data, tables, and figures against source documents before finalization. |
| "Data Dump" Reporting: Presenting tables and figures without a clear narrative to explain their clinical significance. | Pre-Planned Narrative: Develop a narrative strategy and key messages with the full clinical team before writing begins to ensure a consistent, compelling story. |
| Vague Deviation Reporting: Glossing over protocol deviations or failing to analyze their impact on study integrity. | Transparent Deviation Analysis: Maintain a comprehensive deviation log and provide a detailed analysis in the CSR for each significant deviation, explaining its potential impact. |
| Inconsistent Terminology: Using different terms for the same event or concept across the CSR and its appendices. | Controlled Vocabulary: Establish and enforce a study-specific glossary or style guide to ensure all terminology is used consistently throughout all documents. |
| Ignoring Negative Results: Focusing only on positive findings while downplaying or omitting results that don't support the primary hypothesis. | Balanced Interpretation: Present a fair and balanced discussion of all findings, including unexpected or negative results, and discuss their clinical implications. |
Avoiding these traps is about building trust with regulators and presenting research with clarity and integrity. Modern document management and authoring tools can help automate validation and reduce manual QC effort, making these best practices more achievable.
Adapting Templates for Different Study Types
A standardized clinical study report template provides the foundational blueprint based on ICH E3 guidelines. However, this framework is not rigid; it must be adapted to suit the unique characteristics of each clinical trial. The skill lies in tailoring the core template to tell the specific story of the study, ensuring the final report is both compliant and scientifically insightful.
Tailoring the Report for Each Clinical Trial Phase
The scientific questions addressed in a clinical development program evolve from phase to phase. The CSR must reflect these evolving objectives.
-
Phase 1 Studies: The primary focus is safety, tolerability, and pharmacokinetics. The CSR template should emphasize the Safety Evaluation (Section 12) and include detailed pharmacokinetic analyses. Efficacy is typically exploratory and reported as such.
-
Phase 2 Studies: These studies explore dose-response, efficacy, and safety in a target patient population. The template must give balanced weight to the Efficacy Evaluation (Section 11) and the Safety Evaluation (Section 12), with detailed sections for analyzing dose-ranging data.
-
Phase 3 Studies: These are pivotal, confirmatory trials designed to demonstrate a product's benefit-risk profile for a marketing application. The CSR is an extensive document requiring comprehensive information across the Investigational Plan (Section 9), Efficacy Evaluation (Section 11), and Safety Evaluation (Section 12) to support the application.
Adjusting for Therapeutic Area and Study Design
Beyond the trial phase, the specific therapeutic area and study design necessitate further customization. The global clinical trials market—valued at USD 59 billion and projected to reach USD 98.9 billion by 2034—encompasses a vast range of research, each with unique endpoints and data requirements. More details are available in this analysis of the clinical trials market landscape.
For example, oncology trials, which comprise a significant portion (38.4%) of the market, involve complex endpoints like progression-free survival and overall survival, alongside detailed reporting of adverse events associated with cytotoxic agents. A vaccine trial would focus on immunogenicity data and specific reactogenicity events. A medical device study would require unique sections on device performance, usability, and malfunctions not found in a typical pharmaceutical trial template.
Effective master templates are designed with modularity in mind. They often include optional sections or annexes that can be activated or customized based on the specific needs of the trial. This approach ensures regulatory compliance without sacrificing scientific clarity.
Adapting for Integrated Summaries and Post-Market Studies
The ICH E3 structure is a versatile framework that can be adapted for broader regulatory submissions beyond single-study reports.
-
Integrated Summaries of Safety (ISS) and Efficacy (ISE): When pooling data from multiple trials for a marketing application, the CSR template structure can be adapted for these summary documents. This provides a familiar, logical flow for presenting pooled analyses, making the extensive data easier for regulators to navigate.
-
Post-Authorisation Safety Studies (PASS): After a product is marketed, PASS may be conducted to further evaluate its safety profile in a real-world setting. A CSR template for a PASS will be heavily weighted toward safety evaluation and may incorporate methodologies for analyzing observational data, which differ from those used in controlled clinical trials.
Frequently Asked Questions About CSR Templates
This section addresses common practical questions that arise during the preparation of a Clinical Study Report.
What’s the Difference Between a CSR Template and a Synopsis?
The CSR template is the complete structural blueprint for the entire report, outlining all 16 sections mandated by the ICH E3 guideline.
The synopsis is a single component of that blueprint—Section 2. It is a brief, high-level summary of the trial (typically a few pages) that covers the study's design, methods, and principal results.
Regulators often review the synopsis first to gain an overview of the study before conducting a detailed review. While the synopsis is critical for making a strong first impression, the template is the tool that ensures the entire comprehensive report is structured correctly and is complete.
How Do You Handle Protocol Amendments in a CSR Template?
Protocol amendments are a routine part of clinical trials and must be handled systematically in the CSR. A well-designed template will include a dedicated subsection, typically within Section 9 (Investigational Plan), for documenting all protocol amendments.
This section should provide a chronological list of amendments, including for each:
- The version number and date of the amendment
- The date of IRB/IEC approval
- A brief summary of the changes made
Beyond listing them, the impact of these changes must be described in the relevant sections of the report. For example, if an amendment modified the statistical analysis plan, this change and its rationale must be clearly explained in both the methods and results sections to ensure a transparent audit trail.
Can I Use the Same CSR Template for Both FDA and EMA Submissions?
Yes. The purpose of the ICH E3 guideline is to provide a harmonized, internationally accepted standard for CSRs. A single, robust clinical study report template built on ICH E3 is designed to be suitable for submissions to both the FDA and the EMA, as well as other regulatory authorities that have adopted ICH guidelines.
Using the ICH E3 structure ensures that the template includes the sections and information expected by both agencies. While one region may occasionally request specific supplementary information, this can typically be included in an appendix without altering the core structure of the report. This standardization provides significant efficiencies for global submission programs.
Who Is Ultimately Responsible for Approving the CSR?
The final approval of the Clinical Study Report rests with the trial’s sponsor. While the preparation of a CSR is a multidisciplinary team effort, the sponsor’s final signature signifies that the document is a complete, accurate, and official account of the study, ready for regulatory submission.
The core team involved in its preparation includes:
- Medical Writers who draft the narrative and integrate data.
- Biostatisticians who provide and verify the statistical analyses and data displays.
- Clinical Scientists who provide medical context and interpret the findings.
- Data Managers who confirm the consistency of the report's data with the final clinical database.
This team completes numerous review cycles. However, the ultimate accountability lies with an authorized representative of the sponsor organization, who provides the final approval, formally attesting to the report's accuracy and integrity.